Article by John Miller
Muscle Strain Injuries: Recovery Time and Rehabilitation Options
How Long Does It Take For A Muscle Injury To Heal?
Muscle injuries are a common occurrence, and the duration of recovery varies depending on the severity of the injury. Muscle strains can range from mild to severe, with more severe strains requiring longer recovery periods. In some cases, surgical repair and post-operative physiotherapy may be necessary for a full recovery.
It is essential to seek professional assessment and guidance from a physiotherapist to ensure that your injury is treated correctly. They can provide you with specific instructions to aid in your rehabilitation and prevent re-injury.
To assist with your muscle strain rehabilitation, your physiotherapist may use a range of treatments. Acute muscle strain treatment options include early injury treatment, avoiding the HARM factors, using a brace or support, a TENS machine, and soft tissue massage. Subacute muscle strain treatment options may include acupuncture and dry needling, kinesiology tape, supportive taping and strapping, and heat packs. Medications may also be prescribed.
Later stage muscle strain treatment options may include foam rolling, stretching exercises, strength exercises, closed kinetic chain exercises, eccentric exercises, neurodynamics, proprioception and balance exercises, agility and sport-specific exercises.
Other factors to consider in muscle strain rehabilitation include biomechanical analysis, joint mobilisation techniques, gait analysis, running analysis, video analysis, prehabilitation, and yoga.
It is crucial to remember that the information provided in this article is general and should not be used as individual treatment advice. It is recommended that you seek professional guidance from a physiotherapist to receive appropriate treatment for your muscle strain injury.
Muscle Strain Rehabilitation Options
The following options are available to your physiotherapist to assist in rehabilitating your muscle strain. Please seek their professional advice before self-managing your injury to avoid aggravating your muscle strain. These are general guidelines only and should not be treated as individual treatment advice.
Acute Muscle Strain Treatment
Subacute Muscle Strain Treatment
- Sub-Acute Soft Tissue Injury Treatment
- Acupuncture and Dry Needling
- Soft Tissue Massage
- Kinesiology Tape
- Supportive Taping & Strapping
- Electrotherapy & Local Modalities
- Heat Packs
- Medications?
Later Stage Muscle Strain Treatment Options
- Foam Roller
- Stretching Exercises
- Strength Exercises
- Closed Kinetic Chain Exercises
- Eccentric Exercises
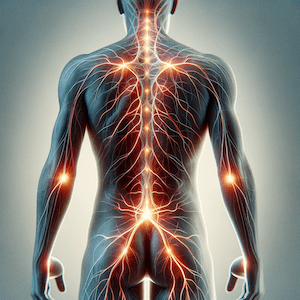
- Neurodynamics
- Proprioception & Balance Exercises
- Agility & Sport-Specific Exercises
Other Factors to Consider
- Biomechanical Analysis
- Joint Mobilisation Techniques
- Gait Analysis
- Running Analysis
- Video Analysis
- Prehabilitation
- Yoga