Flat Feet (Pes Planus)
Article by John Miller
Flat Feet (Pes Planus): Causes, Symptoms, and Physiotherapy Treatment
What are Flat Feet?
Flat feet, also known as pes planus, is a condition where the arch of the foot collapses, causing the entire foot to come into contact with the ground. This can lead to the foot pronating inward excessively, a condition often referred to as overpronation. While some people with flat feet experience no discomfort, others may face challenges due to the altered foot mechanics.
Why Do Flat Feet Occur?
Flat feet can either be congenital, present from birth, or acquired later in life. Congenital flat feet are often a result of inherited traits, with certain ethnic groups more predisposed to this condition. Acquired flat feet typically result from weakened foot and ankle muscles, ligamentous laxity, or excessive weight-bearing activities that cause the arch to collapse.
How Do Flat Feet Progress?
As flat feet progress, they can lead to various complications, particularly if you are physically active. Overpronation can change how forces are distributed through your legs, potentially causing stress fractures or conditions like shin splints. The altered biomechanics of your feet can also lead to deformities, such as bunions, due to abnormal pressure on the bones.
What Complications Can Arise from Flat Feet?
Without proper management, flat feet can lead to several conditions:
- Tibialis Posterior Tendinopathy: This condition occurs when the tibialis posterior muscle, essential for arch stability, becomes overworked and injured.
- Plantar Fasciopathy: Often known as plantar fasciitis, this condition arises from the strain on the plantar fascia due to overpronation.
- Medial Tibial Stress Syndrome (Shin Splints): Overpronation can stress the tibia, leading to shin splints or, in severe cases, stress fractures.
- Achilles Tendinopathy: Flat feet can cause abnormal strain on the Achilles tendon, leading to tendinopathy.
- Patellofemoral Pain Syndrome: The altered mechanics of your foot can affect your kneecap’s movement, causing anterior knee pain.
To discover more, simply click on the links above.

How are Flat Feet Diagnosed?
Diagnosing flat feet typically involves using the Foot Posture Index (FPI), which assesses your foot’s posture from various angles. A comprehensive evaluation by a physiotherapist may include observing your dynamic foot control during weight-bearing activities, as flat feet often cause problems during activities that involve standing or walking. In some cases, a weight-bearing X-ray may be necessary to assess the integrity of the foot’s joints under stress.
Read more: Foot Posture Index
What are the Treatment Options for Flat Feet?
- Restore Muscle Control and Foot Arch Biomechanics: Strengthening the intrinsic muscles of your foot is key to improving arch stability and preventing overpronation. Exercises focused on these muscles can help correct foot mechanics. Read more: Foot Arch Exercises.
- Dynamic Foot Posture Exercises: Addressing any deficiencies in dynamic foot control is essential. A physiotherapist can guide you through exercises to restore proper biomechanics and strengthen the foot’s stabilisers.
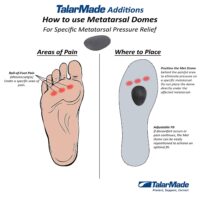
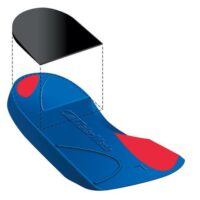
- Orthotics: Temporary or custom-made orthotics may be recommended to provide additional arch support. While most people with flat feet do not require permanent orthotics, they can be beneficial in some cases. Read more: Orthotics
- Restore Calf & Leg Muscle Control: Strengthening the muscles of your leg is crucial for controlling your foot arch and ankle position. Your physiotherapist will provide exercises to address any muscle imbalances.
- Improve Running and Landing Technique: If flat feet affect your sport or work, a physiotherapist can assess and correct your running and landing techniques to prevent further injury. Read more: Running Analysis
- Return to Sport or Work: Tailored exercises will help you return to your activities safely. This may include sport-specific or work-specific training to ensure your flat feet do not interfere with your daily life.
- Footwear Analysis: Wearing the right shoes is vital in managing flat feet. Your physiotherapist can advise you on the best footwear to support your arches and reduce discomfort.
Read more: Orthotics for Flat Feet
Latest Research
Recent studies have highlighted the benefits of specific exercises and orthotics in managing flat feet. A systematic review by Hara et al. (2023) found that targeted strengthening exercises combined with custom orthotics significantly improved foot function in individuals with flat feet. Brijwasi & Borkar (2023).
Read more: New Research on Flat Feet
What to Do?
If you’re experiencing discomfort from flat feet, seek professional advice from your physiotherapist. Early treatment can help prevent complications and maintain an active lifestyle.
Rochedale - Call 38410277
Book Online: RochedaleSalisbury - Call 32751044
Book Online: SalisburySandgate - Call 32691122
Book Online: SandgateRelated Articles
- Bunion Management And Treatment Options: Discusses various foot conditions including bunions, providing insight into their management.
- Anterior Ankle Impingement: Offers a guide on causes, treatments, and tips for anterior ankle impingement, relevant for understanding related ankle issues.
- Ankle Pain: Effective Management And Treatment Options: Explores different causes of ankle pain and provides treatment options, emphasizing the importance of addressing biomechanical issues like flat feet.
- Heel Pain: Investigates causes of heel pain, linking conditions such as plantar fasciitis and heel spurs to flat feet, thus offering a comprehensive look at foot pain sources.
- Plantar Fasciitis: Specifically targets plantar fasciitis, detailing its relationship with flat feet and providing insights into treatment and prevention.
- Metatarsalgia: Examines the pain in the ball of the foot, known as metatarsalgia, discussing how foot biomechanics, including flat feet, can influence such conditions.
- Foot Pain: Provides an overview of common sources of foot pain, including biomechanical conditions like flat feet, and suggests possible treatments.
- Tibialis Posterior Tendinopathy: Explains the role of the tibialis posterior in foot stability and how to manage related issues.
- Achilles Tendinopathy: Discusses the causes and treatments of Achilles tendon issues, often related to flat feet.
- Patellofemoral Pain Syndrome: Examines how flat feet can lead to knee pain and ways to manage it.
- Flat Feet: Offers a comprehensive overview of flat feet, including symptoms and treatment options.
- How to Fix Flat Feet: Provides actionable advice on exercises and treatments for flat feet.
- Flat Feet and Fallen Arches: Discusses the causes, symptoms, and treatment options for flat feet.