Juvenile Osteochondritis Dissecans (JOCD)
What is Juvenile Osteochondritis Dissecans?
Juvenile Osteochondritis Dissecans is a condition of the joint surfaces and underlying bone in people who are still growing. Typically seen in children and young people, JOCD is primarily an active youth person’s condition. Changes in the cartilage and underlying bone lead to pain, alterations in movement and ability to compete in their sport. Although higher activity levels are considered a risk factor, you don’t have to be an athlete to have this condition.
Juvenile Osteochondritis Dissecans Stages
There are four general stages of Juvenile Osteochondritis Dissecans
Stage 1: changes or compression of the bone immediately underlying the cartilage (subchondral bone)
Stage 2: partial separation of the subchondral bone, but no movement away from the cartilage
Stage 3: complete separation of the bone from the cartilage, again with no separation
Stage 4: complete separation of the piece of bone, and it comes away from the remaining bone and floats in the joint cavity
There are a variety of different classification systems for JOCD, but none are widely accepted.
What are the Symptoms of Juvenile Osteochondritis Dissecans?
Each joint in our body has cartilage and subchondral bone, and as such, there are a variety of ways that JOCD presents. Juvenile Osteochondritis Dissecans commonly occurs in the knees (about 95% of cases), hips, ankles, elbows, and collarbones, although they may occur in other joints.
Children and young people will complain of:
- Pain, especially during or after activity
- Swelling
- Reduced joint range of motion
- Crepitus (crunchy or popping noises from joints)
What Causes Juvenile Osteochondritis Dissecans?
There are many theories for what causes Juvenile Osteochondritis Dissecans, but it seems to be many various factors coming together to create the ‘perfect storm’ and produce this condition. Over the years, lots of theories have arisen:
- Genetic susceptibility, where there is a history of Osteochondritis Dissecans in the family or other similar joint conditions
- Repeated microtrauma to the area, sporting populations, are at a higher risk.
- Reduced blood supply to the subchondral bone
- Anatomical variations of knee alignment, meniscus types, blood supply
- Biomechanical (movement) inefficiencies due to obesity, reduced strength, impingement etc.
- Uneven bone growth from anatomical variation or growth plate injury
- Joint instability, either structural or dynamic/functional
- Endocrine (hormonal) changes – vitamin D deficiency, human growth hormone deficiency
How is Juvenile Osteochondritis Dissecans Diagnosed?
There aren’t any valid or specific tests to rule in Juvenile Osteochondritis Dissecans. However, physiotherapists can perform a comprehensive examination to rule out all other options. They look to include or exclude injuries or conditions to the surrounding tissues, including systemic illnesses that manifest as joint pain. Usually, diagnosis is mainly made by a comprehensive interview to understand your symptoms, backed up by imaging, e.g. MRI.
Wilson’s test is one test to examine knees for JOCD, but the reliability and validity of this test are unknown for diagnostic purposes. Wilson’s test may monitor your progression throughout your rehabilitation.
Imaging for Juvenile Osteochondritis Dissecans
If your physiotherapist or GP thinks you might have Juvenile Osteochondritis Dissecans, they will send you for scans. A mix of scans determines if JOCD is present in whichever joint you have pain in because of the different types of tissues they show.
X-rays are usually taken from a variety of views. Typically, images are taken from front to back and the side. Other unique aspects aligned with the natural joint gaps may provide more unobstructed views. These depend on which joint is involved, and your doctor, physio and radiologist will be able to determine if any unique views are needed.
MRI is used to view softer tissue involvement, swelling, bone bruising, and any early-stage changes to the joint surface. There is limited use to determine whether any pieces are ‘free-floating in the joint space. A combination of X-ray and MRI are routine imaging.
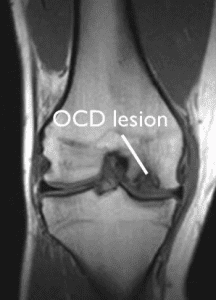
MRI image showing an OCD lesion in a knee (OrthoInfo, 2020)
It would be best if you discussed your Juvenile Osteochondritis Dissecans case with your trusted healthcare professional. Would you please book an appointment with your trusted physiotherapist or doctor?
Treatment Options for Juvenile Osteochondritis Dissecans
Treatment depends on the nature of the changes inside the joint. Your age and whether their growth plates have finished growing are just some of the factors. Joints that don’t have any undisplaced pieces are typically conservatively treated. Treatment options include physiotherapy, reduced loading and a graduated return to activity.
For Juvenile Osteochondritis Dissecans lesions that have fragments or pieces that may come loose into the joint space, please consult your Orthopaedic surgeon’s opinion. They will determine if bone pieces need to be removed or put back into their original place. This removal or salvaging might need to happen before any exercise therapy to avoid further irritation to the inside of the joint surfaces.
Treatment plans are bespoke to each individual, so your physiotherapist and sports physician will discuss your options with you if you have an OCD lesion found on imaging.
Unloader braces have been put forward regarding the knee and elbow OCD to promote healing and maintain movement and independence. Other movement aids like crutches, splints, casts, and different types of bracing are options.
What Results Can You Expect from Juvenile Osteochondritis Dissecans Treatment?
Results vary widely depending on what sort of Juvenile Osteochondritis Dissecans lesion you have, and therefore your treatment.
Conservative treatment:
Pain and swelling management, strengthening, restoration of movement, coordination, and balance retraining are vital components of Juvenile Osteochondritis Dissecans treatment. Treatments focus on returning you to the sport or activity of choice. In the case of no fragment or a fragment that hasn’t moved, conservative treatment commences immediately and typically undergo a 3-6 months trial before deciding if a surgical intervention is needed. As stated above, if there is a loose fragment, your surgeon might need to remove this before starting exercise therapy.
There are no established, widely accepted protocols for conservative treatment. The treatment plans are always bespoke to the person and change over time, depending on their progression. Some guidelines help clinicians to guide a return to weight-bearing. These formulate on your clinician’s experience and consensus statements from leaders in the research.
Critical components of rehabilitation base themselves upon a general phased approach. These phases progress under the guidance of your specialist doctors, surgeons, physios and anyone else collaborating on your treatment team. There is no consensus on what factors guide movement between these phases, but radiographic findings and mechanical symptoms impact. Swelling, pain, neuromuscular control, muscle strength and performance, and weight-bearing are all noted influencing factors.
Surgical treatment:
Outcomes vary widely based on the type of surgery you have. Timelines for treatment and recovery of surgical intervention are best sought from your surgeon if you need operative management. Typically, recovery means six weeks on crutches and 6+ months to get back to full function and return to sport. Your healing includes several months of physiotherapy and exercises rehabilitation to restore movement, strength, coordination and balance. The protocol for this rehabilitation is as per conservative management above.
Stem-Cell Therapy
This type of therapy is in its infancy for OCD. Therefore, it is still too early to determine how effective it is in the long term. Researchers have trilled it in knees, elbows and ankles. There are, however, early, promising results. Currently, its primary use is for those people where surgery has been unsuccessful.
Long Term Outcomes
There is some evidence suggesting that children and young people who suffer from OCD lesions develop osteoarthritis at higher rates than the general population. However, there is a lack of good quality, long-term, well-controlled research. It is challenging to stay just how much of an increased risk there is because much of the research doesn’t allow for considerations like other arthritis risk factors, conservative vs non-operative treatment.
A US research group called the ROCK group research Juvenile Osteochondritis Dissecans in the knee. Their research is ongoing, looking into the different types of surgeries and their outcomes, the long term effects of treatment of JOCD and secondary outcomes/complications. More information will be available when they publish their findings.
For more information, Juvenile Osteochondritis Dissecans is a condition that you must discuss with your trusted physiotherapist or doctor.
Common Youth & Kids Sports Injuries
Rochedale - Call 38410277
Book Online: RochedaleSalisbury - Call 32751044
Book Online: SalisburySandgate - Call 32691122
Book Online: SandgateArticle by John Miller
Youth Leg Injuries: Understanding & Treatment Options
Introduction
Welcome to PhysioWorks' detailed FAQ on Youth Leg Injuries, a resource specifically designed to shed light on leg-related conditions in young individuals. Whether it's sports injuries, overuse conditions, or growth-related issues, our guide covers a wide spectrum of leg injuries that are prevalent among the youth. Each subsection below not only provides insights but also directs you to comprehensive articles for an in-depth understanding, ensuring you're well-informed about these conditions.


Youth Leg Injuries
Young individuals are prone to a variety of leg injuries, each requiring specific attention and care. Our articles focus on identifying symptoms, providing effective treatment options, and offering rehabilitation strategies. Understanding these injuries is vital for a speedy recovery and preventing future complications.
- Osgood Schlatter’s Disease
- Sinding Larsen Johansson Syndrome
- Patellofemoral Pain Syndrome
- Knee Ligament Injuries
- ACL Injury
- Meniscus Tear
- Sever’s Disease
Continue exploring Youth Leg Injuries...
Pelvis & Hip Injuries
Injuries to the pelvis and hip can significantly impact a young person's mobility and sports participation. These articles discuss into various common conditions, their symptoms, and how to manage them effectively.
Discover more about Pelvis & Hip Injuries...
Knee Injuries
The knee, a complex joint, is susceptible to various injuries, particularly in active youths. These resources are tailored to provide information on prevention, diagnosis, and effective treatment for knee injuries.
- Discoid Meniscus
- Osteochondritis Dissecans
- Patella Dislocation
- Osgood Schlatter’s Disease
- Sinding Larsen Johansson Syndrome
- Patellofemoral Pain Syndrome
Read more about Knee Injuries...
Heel & Ankle Injuries
Heel and ankle injuries are common but manageable conditions in youth sports. Our articles cover a range of topics from immediate care to long-term rehabilitation strategies.
Learn more about Heel & Ankle Injuries...
Common Youth & Teenager Sports Injuries
Engaging in sports is beneficial for youths, but it also comes with the risk of injuries. Our resources provide insights into common sports injuries, preventive measures, and effective treatment protocols.
Explore Sports Injuries in Youths...
Conclusion
Understanding and effectively managing youth leg injuries are crucial for their wellbeing and continued active participation in sports and daily activities. This guide, with its extensive resources, aims to equip parents, coaches, and young athletes with the knowledge to handle these injuries confidently. Stay informed and proactive in caring for youth leg health.
Rochedale - Call 38410277
Book Online: RochedaleSalisbury - Call 32751044
Book Online: SalisburySandgate - Call 32691122
Book Online: SandgateRelated Articles
- Avulsion Fracture Recovery: A Physio's Guide - Offers insights into the recovery process for avulsion fractures, a common injury among active youth.
- Osteochondritis Dissecans - Discusses a condition where bone underneath the cartilage of a joint dies due to lack of blood flow, relevant for youth experiencing knee issues.
- Effective Management Of Kids Sports Injuries - Provides a comprehensive guide on handling sports injuries in children, including prevention and treatment strategies.
- Leg Pain - Covers various conditions leading to leg pain and outlines effective treatment strategies, highlighting the role of physiotherapy in pain reduction and mobility improvement.
- Ankle Strapping: Complete Guide To Injury Prevention - Discusses the benefits of ankle strapping as a preventative measure against injuries, focusing on techniques and materials.
- Sinding-Larsen-Johansson Syndrome: Effective Management And Treatment Options - Offers detailed advice on managing conditions leading to SLJ kneecap pain and outlines effective treatment strategies.
- Sever's Disease Explained: Causes, Symptoms, Treatment - Provides an overview of Sever's disease, including common causes, treatment options, and related conditions like plantar fasciopathy and Achilles tendinopathy.
- Osgood Schlatter Disease - Offers insights into the causes, symptoms, and treatment of Osgood-Schlatter disease, a condition causing knee pain.