Article by John Miller
Arthritis Treatment: Taking Action to Improve Your Health
Looking to banish arthritis from your life? The good news is that you have the power to take action right now. From simple one-time steps to long-term strategies, each move you make can directly or indirectly enhance your well-being, outlook, and pain management, making life with arthritis more manageable.
Obtaining an Accurate Diagnosis
When pain, stiffness, or swelling sticks around a joint for over two weeks, it's time to consult your doctor, physiotherapist, or healthcare expert. These symptoms can appear suddenly or creep in gradually. A skilled healthcare professional is the one to determine if arthritis is the culprit. But a mere "you have arthritis" isn't enough. Request a precise diagnosis of the specific type of arthritis you're dealing with. With over 100 types, such as osteoarthritis and rheumatoid arthritis, each requiring distinct treatments, nailing down the right treatment starts with the correct diagnosis.
Shielding Your Joints
Spare your joints from undue stress. Opt for larger or stronger joints when lifting. Task-enhancing tools can simplify activities at home and work. Seek out items bearing the Arthritis Foundation’s Ease-of-Use Commendation – they're comfortable, user-friendly, or thoughtfully packaged. Moreover, maintaining your recommended weight helps alleviate detrimental pressure on your hips and knees.
Keep Moving - Stay Active!
Exercise emerges as a potent weapon to combat pain, enhance mobility, mitigate fatigue, and elevate your overall well-being. A comprehensive exercise regimen for arthritis sufferers encompasses flexibility exercises to expand range of motion, aerobic activities to bolster endurance and reduce fatigue, plus strengthening routines to enhance muscle fitness.
Your physiotherapist can guide you through effective range-of-motion and strength-building exercises tailored for arthritis. The Arthritis Foundation also offers versatile exercise options like aquatic programs, Tai Chi, and walking sessions.
Consistency is key; adults are generally encouraged to engage in a minimum of 2 hours and 30 minutes of moderate-intensity aerobic activity (like brisk walking or gardening) per week, or alternatively, 1 hour and 15 minutes of vigorous aerobic exercise (jogging, aerobic dance). Whether your activity is gentle or vigorous, the objective is to keep those limbs in motion.
Shed Those Extra Kilos
Shedding weight holds benefits beyond just appearances. You’ll feel the difference, too. Why? Every additional kilogram you carry strains your knees and hips. Excess weight equates to more pain, regardless of your arthritis type. It can also exacerbate osteoarthritis and increase your risk of gout.
Boost Your Bone Health
Stock up on calcium-rich sources to fortify your bones. A diet abundant in this vital mineral curbs osteoporosis risk. Additionally, inflammatory arthritis conditions hasten bone loss, underscoring the importance of adequate calcium intake. Recommended daily calcium doses are 1,000 mg for adults below 50 and 1,200 mg for those over 50. If milk isn't your preference, diversify with yogurt, cheese, or ice cream. Other calcium sources include broccoli, bone-in salmon, and kale.
Medications - Handle with Care!
Adhere to your prescribed medication regimen religiously. Before discontinuing due to perceived inefficacy or potential side effects, consult your doctor. Medication benefits might take weeks or months to fully manifest, and certain side effects may wane over time. Abruptly stopping medication can not only deprive you of its advantages but can also pose risks.
Begin Your Day Right
Kickstart your mornings with fruits, fibre-rich foods (like oatmeal), and a refreshing glass of water instead of coffee. A nutritious breakfast sets a positive tone for the day, staving off higher cholesterol, low energy, and overeating tendencies.
Take a Stroll
Select your preferred indoor and outdoor spots, planning a weekly walk. Walking stands as the ideal exercise for most arthritis patients. It torches calories, fortifies muscles, and promotes denser bones without jarring fragile joints.
Relaxation and Relief
Before bedtime, indulge in a warm bath to soothe muscle tension, alleviate achy joints, and foster restful sleep.
Pamper Your Muscles
Treat yourself to a skillful massage from a remedial massage therapist. Benefits may vary but could encompass reduced pain and stiffness, improved circulation, energy, flexibility, and enhanced immune and sleep functions. Mentally, massage can alleviate stress and depression, providing an overall sense of well-being.
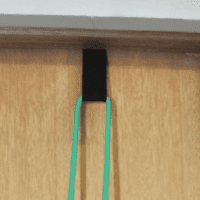
Stretch It Out
Stretching presents a straightforward approach to maintaining joint and muscle flexibility. It eases tension and aids in maintaining daily activities. Strengthen your calf muscles with this simple stretch: Stand a couple of feet from a wall, toes turned inward, palms on the wall. Keep your knees straight and feet flat, lean forward onto your hands without bending at the waist. Feel your calf muscles elongate. Maintain this position for 10 seconds, then gently push away from the wall. Repeat.
Dive In
Certain aquatic programs and exercises suit arthritis patients splendidly. Consider water walking, for instance. Exercising in water enhances strength and range of motion, with water’s buoyancy sparing sore joints from undue strain. Water offers 12 times the resistance of air, furnishing an effective workout without compromising joints.
Embrace the Cold
When joints are inflamed and hot, applying cold compresses can diminish pain and swelling by constricting blood vessels and preventing fluid leakage. Our go-to ice pack: a bag of frozen peas or corn that can mould to your body's contours.
Break Free from Smoking
Challenge yourself to quit smoking, even if for a day, then another, and another. Smoking heightens the risk of complications from conditions like lupus and rheumatoid arthritis. It's linked to higher psoriasis risk and a predisposition to osteoporosis. In cases of joint surgery, smoking can impede recovery. Furthermore, smoking can reduce the effectiveness of arthritis drugs and contribute to sleep disturbances.
Find Enjoyment in Exercise
Transform exercise into an enjoyable endeavour. Enrol in a class that makes staying active a pleasure – think country line dancing, ballroom dancing, swimming, yoga, or Tai Chi. Some of these options offer tailored benefits for arthritis patients. Tai Chi, for instance, alleviates pain and impairment in severe knee osteoarthritis. This slow, graceful practice, initially a Chinese martial art, also diminishes stress and enhances balance. Yoga strengthens and relaxes stiff muscles, aiding in weight loss efforts.
For personalised guidance, consult your physiotherapist or trusted healthcare professional.