Psoriatic Arthritis
Article by Shane Armfield
Psoriatic Arthritis
Understanding and Managing: A Physiotherapist’s Perspective
Introduction
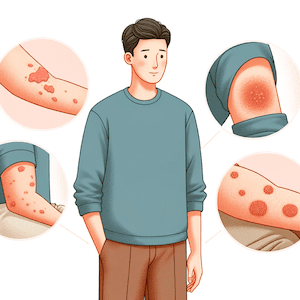
Psoriatic arthritis (PsA) is a chronic inflammatory condition that affects both joints and skin. Typically linked with psoriasis, a skin condition characterised by a red, scaly rash, PsA can significantly impact quality of life. However, with the right approach, including physiotherapy, lifestyle adjustments, and medical treatment, managing PsA effectively is possible. This guide aims to provide a comprehensive understanding of PsA from a physiotherapist’s perspective, emphasising the latest research and management strategies.
What is Psoriatic Arthritis?
Psoriatic arthritis causes painful inflammation in and around the joints. It commonly affects individuals with psoriasis but can also appear before any skin symptoms or without them. The pain arises from nerve irritation due to inflammation and stretching of the joint capsule. When inflammation subsides, the stretched capsule may leave the joint unstable and painful.
Symptoms of Psoriatic Arthritis
The symptoms of PsA can vary but often include:
- Joint pain and stiffness
- Swollen fingers or toes (dactylitis)
- Buttock pain, stiff back or neck (spondylitis)
- Heel pain
- Enthesitis (pain where tendons attach to bones)
- Nail changes (pitting, discolouration, thickening)
- Fatigue
Causes and Diagnosis
The exact cause of PsA is unknown, but a combination of genetic factors and possibly infection are thought to play roles. Overweight individuals are at higher risk. Diagnosis is complex due to varied symptoms and includes physical exams, imaging tests, and blood tests for inflammation markers like ESR and CRP.
Latest Research and Treatment Approaches
Recent research in PsA management highlights the effectiveness of targeted biologic therapies and small molecule medications. These treatments focus on specific parts of the immune system to reduce inflammation and prevent joint damage.
Treatment typically involves:
- Skin treatments with ointments or light therapy
- Medications like NSAIDs, DMARDs, and steroids
- Newer biologic agents and JAK inhibitors
Physiotherapy for Psoriatic Arthritis
Physiotherapy plays a vital role in managing PsA. A physiotherapist can help with:
- Therapeutic exercise to maintain joint mobility and muscle strength
- Heat/cold therapy for pain relief
- Education on managing symptoms
- Acupuncture and manual techniques
- Hydrotherapy for gentle exercise
- Fatigue management
- Splinting advice for joint protection
The Role of Exercise
Exercise is crucial in managing PsA. It helps maintain muscle strength, joint health, and flexibility. Low-impact aerobic activities and progressive resistance training (PRT) are particularly beneficial. Your physiotherapist can tailor an exercise program to your specific needs.
Relaxation Techniques and Mind-Body Therapies
Stress management is essential in PsA. Techniques like guided imagery, muscle relaxation, and mind-body practices (Tai Chi, Pilates, Yoga) can help control symptoms and improve overall well-being.
Self-Management Strategies
- Understanding your condition: Knowledge about PsA empowers you to manage it effectively.
- Activity pacing: Balance activities to avoid overexertion.
- Sleep health: Good sleep hygiene can alleviate symptoms.
- Muscle care: Remedial massage can help reduce muscle stiffness and pain.
- Heat and ice therapy: Apply heat for muscle relaxation and ice for reducing inflammation.
- Aids and equipment: Use supportive devices to reduce joint strain.
When Surgery Is Needed?
In severe cases, surgical interventions like joint replacement or tendon surgery may be necessary. These procedures have high success rates in improving joint function and reducing pain.
Conclusion
Managing Psoriatic Arthritis effectively requires a combination of medical treatment, physiotherapy, and lifestyle adjustments. Understanding the condition, staying active, and using stress-reduction techniques can significantly improve your quality of life.
What to Do?
If you’re experiencing symptoms of Psoriatic Arthritis or have been diagnosed with it, consult a physiotherapist. A tailored physiotherapy plan can help you manage symptoms, maintain joint health, and improve your overall well-being. Consult a healthcare professional to start your journey towards better managing Psoriatic Arthritis.
Rochedale - Call 38410277
Book Online: RochedaleSalisbury - Call 32751044
Book Online: SalisburySandgate - Call 32691122
Book Online: SandgateRelated Articles
- Arthritis & Rheumatology Conditions – Discover the various arthritis and rheumatology conditions that physiotherapy can help manage, offering a broader context for Psoriatic Arthritis within the spectrum of related conditions.
- Heat Packs – Learn how applying heat can help relieve muscle stiffness and pain, a useful self-management strategy for Psoriatic Arthritis symptoms.
- Rheumatoid Arthritis – Although focusing on a different condition, this page provides valuable information on managing arthritis through physiotherapy, which can be relevant for Psoriatic Arthritis sufferers.
- Hand And Wrist Arthritis – Understand how arthritis affects the hand and wrist, including pain management and mobility improvement strategies that can apply to Psoriatic Arthritis.
- Acupuncture and Dry Needling – Explore how these techniques can provide pain relief, a beneficial adjunct to the management plan for Psoriatic Arthritis.
- Soft Tissue Massage – Learn about the benefits of remedial massage for reducing muscle stiffness and pain, supporting the muscle care strategy for Psoriatic Arthritis.
- Strength Exercises – Find out how strength training exercises can help maintain muscle strength and joint health, crucial for managing Psoriatic Arthritis.
- Wrist Brace or Support – This page offers advice on using supportive devices to reduce joint strain, relevant for Psoriatic Arthritis patients experiencing wrist issues.
- Kinesiology Tape – Discover how kinesiology taping can support joints and muscles, potentially beneficial for those with Psoriatic Arthritis.