Trochanteric Bursitis (Hip Bursitis)
Article by John Miller

Trochanteric Bursitis
Managing Hip Bursitis
Trochanteric bursitis stands out as the most prevalent type of hip bursitis, significantly contributing to Greater Trochanteric Pain Syndrome (GTPS). It develops from the inflammation of the bursa, a tiny sac that provides cushioning at points where tendons cross joints.
Specifically, this condition affects the superficial trochanteric bursa, located by the prominent bone on the hip’s side (femur). In more severe cases, a deeper bursa may also become inflamed.
Causes of Hip Bursitis
Typically, repeated compression of the bursa leads to inflammation and pain.
Weakness in the gluteal muscles, notably the gluteus medius, often accompanies this condition, resulting in a Trendelenburg gait pattern, indicative of hip muscle weakness.
GTPS, and subsequently hip bursitis, is more common in females, patients who are overweight or obese, and patients aged 40 to 60 years. It has been suggested that the larger width of the typical female pelvis may cause increased tension on the iliotibial band over the greater trochanter.
Research suggests that inadequately rehabilitated low back pain or hip pathologies can lead to such muscle weaknesses. However, properly tailored exercise protocols focusing on muscle strengthening can effectively reverse this condition. Such exercises should concentrate on individually weak muscles to enhance the strength of gluteal and hip rotator muscles.
Young, active individuals and older adults with gluteal muscle weakness are susceptible to trochanteric bursitis. Activities often linked to this condition include running with poor muscle control, bushwalking to the point of fatigue, and cycling with a high seat causing muscle strain.
Acute cases may arise from falls or sports-related impacts on the hip.
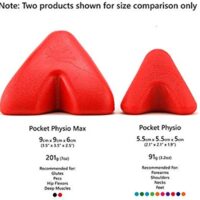
For advice on hip muscle weakness, consulting a physiotherapist experienced in gluteal and hip pathologies is crucial.
Diagnosing Hip Bursitis
Diagnosis typically occurs during a clinical consultation, involving a review of medical history and a physical examination of the hip, pelvis, and back.
Additional diagnostic tools like ultrasound scans or MRI may be employed for confirmation. A key diagnostic indicator is tenderness over the greater trochanter (hip bone) when pressure is applied.
Symptoms
Common symptoms of hip bursitis include:
- Pain and swelling over the side of the hip bone.
- Referred pain travelling down the outer thigh, possibly reaching the knee.
- Discomfort when sleeping on the affected hip or after prolonged sitting.
- Pain during activities such as stair climbing, running, walking, or standing for extended periods.
Seeking advice from a trusted hip physiotherapist or doctor is advisable if these symptoms are present.

Effective Treatments for Trochanteric Bursitis
Treatment strategies include:
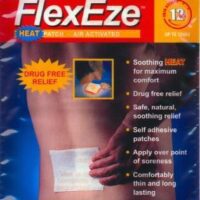
- Early pain relief and anti-inflammatory measures.
- Kinesiology tape to de-load the bursa.
- Corrective exercises targeting specific muscle weaknesses.
- Preventative exercises to reduce future bursa irritation.
- Weight reduction is beneficial.
Anti-inflammatory Agents
When considering anti-inflammatory options, it’s crucial to have a discussion with your doctor. This conversation should cover both NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) and natural anti-inflammatories like arnica. Your doctor’s guidance is essential to prevent potential side effects.
Applying ice packs several times daily can be beneficial. Ice is a natural anti-inflammatory agent that helps reduce pain and swelling.
Corticosteroid Injections for Hip Bursitis
Another effective treatment is a combined injection of a corticosteroid and a local anaesthetic directly into the bursa. This procedure is performed under ultrasound guidance and can significantly decrease inflammation. The local anaesthetic offers immediate pain relief, while the cortisone gradually works over the subsequent days.
Although these injections can alleviate pain, they don’t necessarily address underlying issues like muscle weakness that might have contributed to the bursitis. Therefore, it’s important to also consider corrective and preventative exercises. These exercises are key strategies for preventing recurrence of the condition.
Steroid injections can relieve pain for 3 to 6 months, but individual responses may vary. Steroid injections may be repeated but are limited to 3 or 4 injections per year due to the increased risk of side effects from cumulative steroid administration. (Raythatha M et al 2019)
Phased Treatment Approach
Phase I:
Focuses on alleviating pain and protecting the hip, employing strategies like active rest, ice therapy, and cortisone injections. Treatment techniques may include ice, electrotherapy, acupuncture, de-loading taping techniques, and the temporary use of mobility aids.
Phase II:
Aims to restore normal hip function, including joint range of motion, muscle length, strength, and walking patterns. PhysioWorks’ “Hip Core Stabilisation Program” assists in regaining standard hip muscle control.
Phase III:
The final stage targets returning to desired activities, with rehabilitation tailored to individual functional goals.
Surgery, specifically a bursectomy, remains a rare treatment option for persistent cases.
Expected Results and Prevention
Physiotherapy often yields positive outcomes within weeks, though chronic cases may take longer. Maintaining rehabilitation exercises even after pain subsides is crucial for preventing recurrence. The best prevention strategy includes excellent hip muscle control, guided by your physiotherapist or doctor.
Conclusion
Trochanteric bursitis can restrict your daily activities due to discomfort, but proper treatment and rehabilitation can lead to significant improvements.
Always work closely with your physiotherapist or doctor, adhere to their advice, and continue your exercises to avoid recurrence. If experiencing symptoms of trochanteric bursitis, seek professional help.
Rochedale - Call 38410277
Book Online: RochedaleSalisbury - Call 32751044
Book Online: SalisburySandgate - Call 32691122
Book Online: SandgateRelated Articles
- Greater Trochanteric Pain Syndrome (GTPS): Offers insights into the syndrome that includes hip bursitis as a condition, providing a broader context of hip pain.
- Gluteal Tendinopathy: Discusses causes, symptoms, and treatments of tendinopathy, a condition often associated with hip bursitis, emphasising rehabilitation and prevention.
- Hip Pain Overview: Explains various causes of hip pain, including bursitis, and emphasises the importance of tailored exercise programs for management.
- Bursitis Information: Provides a comprehensive look at bursitis affecting different body parts, useful for understanding the condition in a wider context.
- Hip Flexor: Iliopsoas Groin Pain: Covers causes and treatments for hip flexor pain, which can be related to or exacerbate symptoms of hip bursitis.
- Piriformis Syndrome: Offers treatment tips for Piriformis Syndrome, which can sometimes be confused with or related to hip bursitis due to similar symptomatology in the buttock area.
- Hip Replacement Information: Although more related to end-stage joint disease, it provides context on severe cases and recovery tips that might be beneficial for those with chronic hip bursitis contemplating surgical options.