Rheumatoid Arthritis
Article by Shane Armfield

What is Rheumatoid Arthritis?
Rheumatoid Arthritis is an autoimmune disease that causes inflammation in your joints. The main symptoms are joint pain and swelling. Rheumatoid Arthritis can also be referred to colloquially as Rheumatism and is best treated by a physiotherapist with a particular interest in Rheumatoid Physiotherapy.
Rheumatoid Arthritis causes inflammation in the synovium (covering the joint, which produces a small amount of synovial fluid that nourishes the cartilage and lubricates the joint). A build-up of fluid and cells causes inflammation in the synovium. This results in red and swollen joints that produce extra fluid and pain.
Your joint hurts for two reasons:
- Your nerve endings are irritated by the chemicals produced by the inflammation.
- The swelling stretches the capsule in your joint.
When the inflammation reduces, the capsule remains stretched and can’t hold your joint properly. This can make your joints unstable and move into unusual or deformed positions over time.
What are the Symptoms of Rheumatoid Arthritis?
Rheumatoid Arthritis varies from person to person, but it usually starts quite slowly. Symptoms tend to come and go. You may also have flare-ups when your symptoms become worse than usual.
Common symptoms of Rheumatoid Arthritis include:
- joint pain and swelling (fingers, wrists or the balls of your feet)
- stiffness (morning stiffness lasting over 30 minutes)
- tiredness (fatigue), depression, irritability
- anaemia
- flu-like symptoms, such as feeling generally ill, feeling hot and sweating.
- rheumatoid nodules (fleshy lumps below the elbows or on hands and feet)

How is Rheumatoid Arthritis Diagnosed?
Due to the variety of symptoms experienced by patients, diagnosing Rheumatoid Arthritis can be complex. Doctors will confirm the diagnosis based on your symptoms, a physical examination and the results of x-rays, scans and blood tests. Your doctor may also refer you to a specialist (Rheumatologist) to confirm the diagnosis and receive treatment.
Blood tests, in this case, are used to measure inflammation. You may have one of these tests:
- Erythrocyte Sedimentation Rate (ESR)
- C-Reactive Protein (CRP).
Both of these may show a high value when inflammation is present. These tests may be repeated occasionally to help monitor your arthritis.
Please seek the professional advice of your doctor or physiotherapist.
What’s the Treatment of Rheumatoid Arthritis?
There is currently no cure for Rheumatoid Arthritis, but various treatments can slow down the condition and keep joint damage minimal.
The three main aspects of the treatment of rheumatoid arthritis are:
- Prescribed Drugs
- Rheumatology Physiotherapy
- Surgery
Physical Therapies for Rheumatoid Arthritis
Looking after your joints and managing your symptoms is very important in treating Rheumatoid Arthritis. Your physiotherapist can suggest several different therapies that may help ease your symptoms and reduce the impact Rheumatoid Arthritis can have on your life.
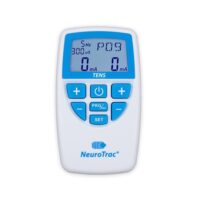
The following treatments have been shown to help patients with Rheumatoid Arthritis.
- Therapeutic Exercise
- Heat/Cold Therapy
- Education
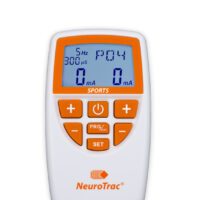
- Pain Management
- Acupuncture
- Splinting Joints
- Fatigue management
- Manual techniques
- Hydrotherapy
Drugs for Rheumatoid Arthritis
Four main groups of drugs are used to treat Rheumatoid Arthritis:
- painkillers (analgesics)
- non-steroidal anti-inflammatory drugs (NSAIDs)
- disease-modifying anti-rheumatic drugs (DMARDs)
- steroids.
Your doctor or rheumatologist is the best clinician to discuss these drugs with and will manage the use of these medications carefully.
Surgery
Surgery is occasionally needed for rheumatoid arthritis. These may include injections, tendon surgery or, in extreme cases, joint replacement. The outcomes of these procedures are successful.
Professional healthcare advice is highly recommended.
What Can You Do For Yourself?
Understand your condition and how it affects you.
- “Knowledge is power”. Educating yourself on the condition will help you manage your symptoms better and empower you to talk to others (Rheumatologist, GP, family etc.) about your situation.
- Self-management courses – can help you build skills and confidence in becoming more actively involved in your healthcare and managing rheumatoid arthritis day today.
- Knowing about your medications can help you and your medical provider manage your symptoms more effectively.
- Understanding how your behaviour and activities influence your symptoms can help you reduce the pain and suffering caused by RA. Speaking to a health professional can help you identify aspects of your life that may be aggravating your RA and help address them.
Keep Moving – But Respect Your Pain & Swelling
- Exercise helps to lessen your pain in the long run by maintaining muscle strength and optimising joint health.
- Well-designed activity programs can increase your range of movement, reduce fatigue and help you feel better overall.
- Appropriate low-impact aerobic activities like hydrotherapy, cycling, Tai chi, pilates and walking can help improve your general health and manage your symptoms.
- A strength-training program called progressive resistance training (PRT) has improved physical function in people with Rheumatoid arthritis.
- Your physiotherapist will assess and prescribe rheumatoid arthritis exercises. Ask them what is best for you.
Relaxation techniques
- Managing stress and anxiety with muscle relaxation techniques, distraction, guided imagery, and other techniques can help improve your general health and control painful symptoms.
- Activities such as Tai Chi, Pilates and Yoga are great ways to relax and de-stress while conditioning the muscles and joints in the body.
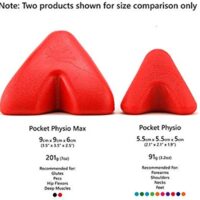
Aids and equipment
- Supports like walking aids and specialised cooking utensils reduce joint strain and help you manage pain and fatigue. Your therapist can give you advice on aids.
Heat and Ice Therapy
- Heat – heat works to reduce muscle tension and stimulate blood circulation. You may find that applying something warm before getting up in the morning or during the day helps reduce discomfort and stiffness in your joints.
- Ice – Ice helps reduce inflammation in muscles and joints by constricting blood vessels and preventing fluids from leaking into surrounding tissues. It would help if you tried icing your joints after any significant activity or at the end of the day. This can minimise the inflammation resulting from daily activities.
Activity Pacing
- Knowing how your daily habits and activities influence your symptoms is very important. Overexertion can increase your pain and symptoms, while underactivity can have similar effects. Learning about activity pacing through diaries and activity management strategies can help you achieve what you want, but with less pain or discomfort.
Sleep Health
- Poor sleep patterns, environment, and position can significantly impact your pain and symptoms. Most people are unaware of the factors that can influence sleep health, so addressing these factors can help you manage your symptoms. A good therapist can assess your sleep health and provide you with aids and education to improve this aspect of your life.
Treat Your Muscles
- A quality remedial massage may be just the relief your muscles need. Treat yourself to a good rub down with someone you trust. The benefits vary from person to person but may include decreased pain and muscle stiffness associated with arthritis, increased circulation, and improved sleep and immune functions. Mentally, massage can also reduce stress and depression. Besides all that, massage feels good!
For more advice, please ask your Rheumatology Physiotherapist, Doctor or Rheumatologist.
Related Articles
- Arthritis Overview – Provides comprehensive information on different types of arthritis, including rheumatoid arthritis.
- Rheumatology Physiotherapy – Offers insights into physiotherapy treatments specifically for arthritis-related conditions.
- Osteoarthritis Information – Discusses osteoarthritis, a condition often confused with rheumatoid arthritis, highlighting the differences and similarities.
- Ankylosing Spondylitis: This page discusses how physiotherapy can help manage symptoms of Ankylosing Spondylitis, including pain relief and stiffness reduction.
- Fibromyalgia – Covers causes and treatments for fibromyalgia.
- Psoriatic Arthritis – Explains psoriatic arthritis and common treatments for this condition.
- Lupus – The page discusses lupus and its treatment options.