Referred Pain

Article by Matthew Hewitt
Referred Pain
Referred Pain: Understanding and Managing This Phenomenon

What is Referred Pain?
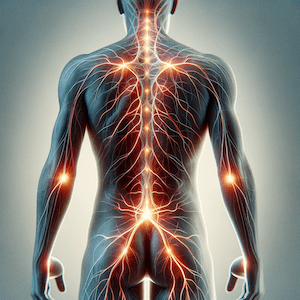
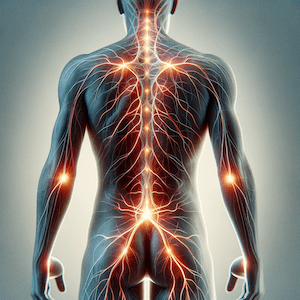
Referred pain is a phenomenon where pain is felt at a location other than where the actual problem is. This can complicate diagnoses and treatment plans, as the source of the pain may be distant from the area experiencing discomfort. Understanding referred pain is crucial for healthcare professionals to diagnose and manage various medical conditions effectively.
Mechanisms of Referred Pain
Referred pain occurs due to the complex interaction between nerves, the spinal cord, and the brain. The primary mechanisms include:
Convergence-Projection Theory
This theory suggests that nerves from different parts of the body converge at the same levels in the spinal cord. When a painful stimulus occurs in one area, the brain may misinterpret the origin of the pain due to overlapping nerve signals, projecting it to another region. Think of this as interference between a stereo and its speakers.
Central Sensitisation
Central sensitisation happens when the central nervous system (brain and spinal cord) becomes sensitised, leading to an increased response to normal sensory inputs. Over time, this can cause pain to be perceived in areas other than where the actual damage or stimulus is located. This often occurs with repeated irritation over time.
Peripheral Nervous System Involvement
Irritation or inflammation in one part of the body can affect the nerves in another part due to shared pathways or close anatomical proximity. This can happen when tissue surrounding a nerve goes into spasm or becomes swollen, compressing the nerve. An example is piriformis syndrome.
Common Examples of Referred Pain
Several medical conditions manifest as referred pain, making it essential to recognise these patterns:
Sciatica
Sciatica is an example of referred pain, where an irritated nerve (often in the lower lumbar spine) causes pain to be felt down the back of the leg. One of the most common signs of sciatica is worsening leg pain with sitting or bending.
Double Crush Syndrome
Double crush syndrome involves referred pain where carpal tunnel symptoms are felt with movements of the head or neck. This occurs due to the nerves in your arm exiting from your lower cervical spine.
Heart Attack (Cardiac Ischemia)
During a heart attack, you may experience referred pain in the left shoulder, arm, neck, or jaw. This happens because of shared spinal segments (C3-T4) between the heart and these regions.
Diagnosis and Management
Diagnosing referred pain requires a thorough understanding of anatomy, nerve pathways, and common referred pain patterns. Healthcare professionals use various strategies to pinpoint the source of pain:
History and Examination
A detailed patient history and a comprehensive physical examination are critical. Understanding the characteristics, onset, duration, and location of pain helps in identifying its source.
Imaging Studies
Techniques such as X-rays, MRIs, CT scans, and ultrasound can visualise internal structures and identify potential pain sources not evident through physical examination alone.
Nerve Block Injections
In complicated cases, your doctor may recommend local anaesthetics to specific nerves to help diagnose referred pain. If the pain is relieved after the injection, it confirms the involvement of that nerve pathway.
Electrodiagnostic Studies
Special tests like electromyography (EMG) and nerve conduction studies (NCS) can assess nerve function and identify abnormalities causing referred pain.
Treatment Strategies
Managing referred pain involves addressing the underlying cause and providing symptomatic relief:
- Manual Therapy: Techniques such as joint mobilisation, soft tissue mobilisation, and myofascial release can alleviate pain and improve function. Ask your physiotherapist for specific advice.
- Therapeutic Exercises: Customised exercises targeting flexibility, strength, and endurance can address the underlying causes of referred pain. Your physiotherapist can assist you.
- Postural Training: Improving ergonomics and posture can prevent the recurrence of referred pain. Ask your physio.
- Neuromuscular Re-education: Retraining the nervous system can reduce central sensitisation and improve motor control. Seek the assistance of your physiotherapist.
- Education and Self-Management: Strategies may include home exercises, lifestyle modifications, and pain management techniques. Specific advice is available from your physiotherapist.
- Modalities: Treatments like ultrasound, electrical stimulation (TENS), and heat/cold therapy can provide symptomatic relief. Check with your physiotherapist first.
- Medications: Analgesics, anti-inflammatory drugs, or nerve pain medications may be prescribed. Your doctor’s advice should be sought.
- Surgery: In rare or severe cases, surgical procedures may be necessary.
Conclusion
Referred pain is a complex phenomenon that requires a multifaceted approach for accurate diagnosis and effective management. By understanding the underlying mechanisms and common patterns, healthcare professionals can better diagnose and treat patients, improving outcomes and alleviating suffering.
What to Do?
If you experience unexplained pain, consult a physiotherapist or doctor. They can help diagnose referred pain and provide tailored treatment plans to address your specific needs.
Rochedale - Call 38410277
Book Online: RochedaleSalisbury - Call 32751044
Book Online: SalisburySandgate - Call 32691122
Book Online: SandgateReferred Pain FAQs
- What is referred pain? Referred pain is pain felt in a different location from the source of the problem, due to nerve signal misinterpretation.
- What causes referred pain? Referred pain is caused by the convergence of nerve signals, central sensitisation, or peripheral nerve involvement.
- How is referred pain diagnosed? Diagnosis involves a detailed history, physical examination, imaging studies, nerve block injections, and electrodiagnostic tests. Book an appointment with your doctor or physiotherapist.
- Can referred pain be treated? Yes, treatments include manual therapy, therapeutic exercises, postural training, neuromuscular re-education, modalities, medications, and, in severe cases, surgery. Book an appointment with your trusted healthcare professional.
- What are common examples of referred pain? Common examples include sciatica, double crush syndrome, and pain from a heart attack referred to the shoulder, arm, neck, or jaw.
- When should I see a physiotherapist for referred pain? Consult a physiotherapist if you have unexplained pain, especially if it’s persistent or affects your daily activities.
Related Articles
- Sciatica Treatment
- Discover effective treatments for sciatica and ways to manage symptoms.
- Neck Pain Treatment
- Learn about various causes of neck pain and treatment options.
- Shoulder Pain Treatment
- Explore the causes of shoulder pain and physiotherapy solutions.
- Heart Attack Symptoms
- Understand the symptoms of a heart attack and the importance of timely intervention.
- Piriformis Syndrome
- Find out more about piriformis syndrome and how to manage it.
- Carpal Tunnel Syndrome
- Learn about the causes, symptoms, and treatments for carpal tunnel syndrome.
- Low Back Pain Treatment
- Get insights into treating and managing low back pain.
- Postural Training
- Discover how improving posture can prevent pain and improve overall health.
- Manual Therapy Techniques
- Explore various manual therapy techniques used in physiotherapy.
Article by John Miller
What is Pain?
Pain is a critical signal from the body indicating injury or distress. Whether you experience acute or chronic pain, understanding its nature is the first step towards effective treatment. This FAQ page, from a physiotherapist’s perspective, will explain the types, causes, and treatments for various pain conditions.
Why does pain occur?
Pain occurs when nociceptors, specialised nerve cells, detect harmful stimuli such as heat, pressure, or chemical changes. These receptors trigger a series of signals through nerve fibres to the brain, where they are interpreted as pain. This response serves as an alert system, helping us avoid further injury.
How is pain transmitted in the body?
The transmission of pain signals begins with receptor nerve cells at the site of injury. These signals travel via nerve fibres (A-beta, A-delta, and C fibres) through the spinal cord to the brain. The speed and type of nerve fibres involved influence the nature of pain—whether sharp, acute, or chronic.
What is the difference between acute and chronic pain?
Acute pain typically occurs suddenly due to injury or illness and resolves as the body heals. Chronic pain, however, lasts longer than three months, often persisting even after the original injury or illness has healed. Chronic pain can involve complex interactions between the nervous system and psychological factors.
More info: Chronic Pain Explained
How can physiotherapy help in managing pain?
Physiotherapy uses a combination of manual therapy, tailored exercises, and education to manage pain. Techniques like joint mobilisation, massage, and specific exercise programs improve muscle strength and flexibility, reducing pain and preventing further injuries.
Physiotherapy generally focuses on non-invasive, drug-free methods for managing pain and improving function. However, in some cases, pharmacological intervention, such as pain relievers or anti-inflammatory medications, may be recommended alongside physiotherapy. This is typically decided by a doctor or pharmacist and is used to manage acute or chronic pain, allowing patients to engage more effectively in physiotherapy exercises. Common medications may include NSAIDs (non-steroidal anti-inflammatory drugs), muscle relaxants, or nerve pain medications.
Learn more about physiotherapy treatments for pain
What is nerve pain, and how is it treated?
Nerve pain (neuropathic pain) is caused by damage or irritation to the nerves and can feel like shooting, burning, or stabbing sensations. Physiotherapy can help manage nerve pain through exercises, manual therapy, and education on nerve mobilisation techniques.
Discover more about nerve pain management
What role does the brain play in pain perception?
The brain plays a significant role in interpreting pain signals. It processes sensory input from nerve cells and can even modulate the intensity of pain based on psychological and emotional factors, which is why pain can feel worse under stress or anxiety.
Can stress or anxiety worsen physical pain?
Yes, stress and anxiety can significantly impact the perception of pain. When stressed, the body releases hormones like cortisol, which can heighten the sensitivity to pain. Additionally, anxiety can lead to muscle tension, which may aggravate existing pain conditions. Managing stress through relaxation techniques, exercise, and cognitive behavioural therapy (CBT) can help reduce the impact of stress on pain.
What can I do at home to manage pain?
Home-based strategies to manage pain include applying ice or heat, engaging in gentle exercise, and practising relaxation techniques such as deep breathing or meditation. Physiotherapists can provide personalised home exercise programs to improve mobility and reduce pain.
Conclusion
Pain, whether acute or chronic, impacts every aspect of life. With tailored physiotherapy techniques such as manual therapy, exercise, and education, pain can be managed effectively. Seek a doctor or physiotherapist's guidance for a personalised pain management plan.
Rochedale - Call 38410277
Book Online: RochedaleSalisbury - Call 32751044
Book Online: SalisburySandgate - Call 32691122
Book Online: SandgateRelated Articles
- Chronic Pain – Discover effective physiotherapy treatments for chronic pain.
- Nerve Pain – Learn about the causes of nerve pain and how to manage it.
- Post-Exercise Muscle Soreness – Understand why your muscles hurt after exercise and how to prevent it.
- Pain Management – Explore physiotherapy techniques for managing various types of pain.
- Spinal Pain – Learn about spinal pain causes and treatment options.
- Back Pain Relief – Discover effective ways to alleviate back pain.
- Joint Pain – Find out how physiotherapy can help with joint pain.
- Manual Therapy – Learn about hands-on techniques to relieve pain.
- Exercise for Pain Relief – Find out how specific exercises can manage chronic pain.
- Massage Therapy – Learn how massage therapy can alleviate muscle and joint pain.
- Understanding Chronic Pain: Causes and Treatments – Discusses the complexities of chronic pain and its management options.
- Nerve Pain Relief: Best Practices – Offers insights into managing nerve pain with both medication and physiotherapy techniques.
- Physiotherapy and Pain Management – Explains the role of physiotherapy in addressing both acute and chronic pain.
Follow Us for Free Tips
Stay updated with the latest tips on managing pain by following us on social media. Our team regularly shares valuable insights to help you stay pain-free and healthy. Follow us on Facebook, Instagram, and Twitter to get expert advice and physiotherapy tips tailored to your needs.















































