Staying Well
Staying well doesn’t always look the same for each person and will rarely ever be a straight line. It’s important to note that injury and illness cannot be avoided entirely, though we can have an impact on what we do when it does happen. This page outlines the process of ‘Staying Well’ after injury or illness and provides sources and information to find the right professional help for you.
See:

Mental Health Support for Injury Recovery
The psychological impact of injury can often surpass the physical toll itself. Whether sustained at work or during sports, the urgency to return to normal activities can result in incomplete healing rather than full recovery. Tasks once performed effortlessly may become daunting; for instance, footballers may find their technique altered, while construction workers may struggle with lifting heavy objects.
The persistent awareness of lost capabilities can significantly burden one’s mental state, compounded by the fear of re-injury that often deters individuals from resuming their previous routines. This mental struggle is frequently underestimated, yet varies widely from person to person and across different types of injuries.
Addressing mental health changes during recovery is crucial, as declining ability to engage in work, recreational pursuits, or daily tasks can exacerbate existing mental health issues. Recognizing and managing these challenges early on is essential for fostering effective rehabilitation and overall well-being.

Coping with Pain
Understanding different types of pain (please see: Understanding & Managing Pain) can improve our ability to cope with pain, where further understanding can change our mindset. As mentioned in the page about understanding and managing pain, our pain experience can differ based on physical, emotional and mental states.
Pain management can be dealt with in many ways, often individualized and tailored to suit each person and their needs. Professional help is needed in each situation where recent studies emphasize the importance of a holistic approach to pain management, incorporating physical therapy, lifestyle modifications, and psychological support. Physiotherapists and Exercise Physiologists play an important role in helping individuals
understand what ‘good pain’ or ‘bad pain’ may be. Because pain is more a psychological response over a physical one, identifying when pain can be accepted and when to stop is a large part of rehab.
Seeking professional support to help work with/through chronic pain is important as many people will not know where to start and avoid all pain-inducing activities. It is important to note that some pain is expected through physical activity and therapy, and it is important to find professional advice to work through what pain is and is not safe.
Seeking Professional Support
When recovering from injury, it’s common to consult various specialists such as physiotherapists, exercise physiologists, and surgeons to aid in physical healing and pain management. Similarly, prioritizing mental health support is crucial during this journey. While physiotherapists and exercise physiologists often have insights into managing both physical and emotional aspects of pain, psychologists or mental health-trained exercise physiologists specialize in addressing specific mental health issues that may arise from injury and recovery.
It’s advisable to seek professional guidance early in your recovery process to address any mental health challenges effectively. There are several therapeutic approaches beneficial for managing injury-related psychological issues, tailored to individual needs and preferences. A comprehensive assessment by a qualified mental health professional can determine the most suitable therapy, including:
1. Cognitive Behavioural Therapy (CBT): Focuses on changing negative thought patterns and behaviours to alleviate emotional distress and improve coping mechanisms related to injury.
2. Acceptance and Commitment Therapy (ACT): Combines mindfulness techniques with strategies to help individuals accept difficult emotions while committing to actions aligned with personal values.
3. Mindfulness-Based Stress Reduction (MBSR): Teaches mindfulness practices to cultivate present-moment awareness, reducing stress and enhancing overall well-being during recovery.
4. Exposure Therapy: Gradual exposure to injury-related situations to reduce fear and avoidance behaviours, aiding in processing traumatic experiences in a controlled setting.
5. Group Therapy: Provides a supportive environment for individuals facing similar challenges, fostering connection, and skill-building under professional guidance.
Psychologists offer therapies such as CBT, ACT, MBSR, and group therapy, while trained Exercise Physiologists can administer exposure therapy for sports-related injuries. It’s important to explore different therapies and health professionals to find what works best for you, as effectiveness can vary among individuals and providers.
For additional mental health resources and support, Queensland Health provides valuable information. You can also contact the Australian Counselling Association at 1300 784 333 for counselling services or the Australian Psychological Society at 1800 333 497 to connect with a psychologist. Use the Lifeline service finder to locate other free or low-cost health and community services in your local area.
Please see ‘Preventing Future Injuries’ for further information regarding rehabilitation if needed.

Preventing Future Injuries: Ensuring Long-Term Health and Performance
Understanding the Impact of Past Injuries:
Preventing future injuries is crucial for maintaining ongoing health and the ability to participate fully in work and recreational activities. Repetitive injuries at the same site can lead to permanent disability or dysfunction, and they often have cumulative psychological effects. While many people might think that avoiding the activity that caused the injury is the best prevention, it’s more effective to learn from past injuries with the guidance of an exercise professional. They can help individuals return to activities with a holistic approach, addressing the root cause of the initial problem and ensuring the body is stronger and better prepared than before.

Importance of Preventing Future Injuries
Preventing future injuries is paramount for several reasons:
1. Maintaining Physical Health: Each injury increases the risk of complications or chronic conditions. Prevention allows individuals to sustain physical health, engage in daily activities, and maintain independence.
2. Reducing Pain and Discomfort: Injuries often cause significant pain and discomfort, impacting quality of life. Prevention minimizes the risk of additional pain and suffering.
3. Preserving Functionality and Mobility: Injuries can result in temporary or permanent loss of function and mobility. Prevention helps preserve individuals’ ability to move freely and perform daily tasks without limitations.
4. Preventing Disability: Severe injuries can lead to disability, affecting work, social activities, and relationships. Prevention reduces this risk, maintaining independence.
5. Improving Mental Health: Dealing with injury-related physical and emotional consequences can strain mental health. Prevention reduces stress, anxiety, and depression associated with injury and recovery challenges.
6. Lowering Healthcare Costs: Injuries require medical treatment, rehabilitation, and sometimes surgery, which can be costly. Prevention reduces healthcare expenses for individuals and systems.
7. Enhancing Quality of Life: Preventing injuries contributes to a higher quality of life, allowing individuals to enjoy activities, pursue goals, and maintain well-being.
8. Promoting Longevity: Chronic injuries and health conditions can shorten lifespan. Prevention supports longevity by maintaining physical health and reducing complications.
9. Maintaining Productivity: Injuries can lead to work absence or reduced productivity, impacting careers and financial stability. Prevention supports ongoing productivity and economic well-being.
10. Empowering Individuals: Taking proactive steps to prevent injuries empowers individuals to manage their health, fostering resilience and confidence.
Understanding Risk Factors
Injuries result from various factors such as poor conditioning, inadequate warm-up, overtraining, and biomechanical issues. Many injuries are preventable with proper training progression, technique correction, and individualized assessments by professionals like physiotherapists, exercise physiologists, and surgeons.
Importance of Warm-up and Cool-down Routines
Warm-up Benefits:
– Physical Preparation: Increases muscle temperature, blood circulation, joint flexibility, and activates the nervous system, enhancing performance and reducing injury risk.
– Mental Preparation: Prepares athletes mentally for activity, focusing on technique, strategy, and goals.
– Psychological Benefits: Boosts confidence, reduces anxiety, and establishes pre-game rituals for consistency and control.
– Long-term Health: Contributes to overall fitness and well-being, supporting athletic longevity.
Cool-down Benefits:
– Gradual Return to Resting State: Prevents sudden drops in heart rate and blood pressure, reducing dizziness or fainting.
– Blood Flow Redistribution: Prevents pooling in extremities, aids in waste product removal, and reduces muscle soreness.
– Muscle Repair and Growth: Supplies nutrients for recovery, enhancing adaptation to training.
– Injury Prevention: Maintains joint mobility, flexibility, and identifies areas needing attention before the next session.
– Psychological Benefits: Promotes relaxation, reduces stress, and supports mental well-being post-exercise.

Lifestyle Modifications
Lifestyle adjustments such as nutrition, hydration, adequate rest, and recovery are critical for injury prevention. They optimize physical readiness and reduce the risk of overtraining injuries. These adjustments can be assisted by dieticians, exercise scientists and exercise
physiologists. Speaking to a professional about your recovery is important to get the correct information.
Proper Form and Technique
Using correct form and technique minimizes injury risk during physical activity. Proper exercise execution and gradual intensity increase are essential for safety and effectiveness. It is often that increasing weight or reps too quickly puts the body under too much stress which will lead to eventual injury. Progressive loading and exposure to different stimuli to build stability and gradual strength within the whole muscular system is important to keep the whole system healthy.
Regular Physical Assessments
Regular assessments by fitness professionals or physical therapists identify imbalances, weaknesses, or movement dysfunctions. They help develop personalized injury prevention programs tailored to individual needs.
Incorporating injury prevention strategies into daily routines is essential for long-term health, performance, and well-being. It enables individuals to live actively and pursue their passions without the setbacks of preventable injuries. By understanding risk factors, implementing warm-up and cool-down routines, and making lifestyle adjustments, individuals can effectively minimize injury risks and maintain their physical and mental health over time. Keeping regular contact with a fitness professional
Role of AEP’s in Preventing Future Injuries
Accredited Exercise Physiologists (AEPs) play a crucial role in preventing future injuries through their expertise in exercise prescription, biomechanics, and injury prevention strategies. Here’s how an AEP can help:
1. Comprehensive Assessment:
– AEPs conduct thorough assessments of an individual’s physical fitness, movement patterns, and medical history to identify any existing injuries, weaknesses, or imbalances.
– By understanding a client’s specific needs and limitations, AEPs can tailor exercise programs to address areas of concern and reduce the risk of future injuries.
2. Individualised Exercise Programs:
– Based on the assessment findings, AEPs design personalized exercise programs that focus on improving strength, flexibility, balance, and overall functional capacity.
– These programs are tailored to the individual’s goals, preferences, and current fitness level, ensuring safe and effective progression over time.
3. Corrective Exercise Techniques:
– AEPs utilize corrective exercise techniques to address movement dysfunctions, muscle imbalances, and faulty biomechanics that may contribute to injury risk.
– Through targeted exercises and movement re-education, AEPs help clients improve their posture, alignment, and movement mechanics to prevent injuries during physical activity.
4. Education and Empowerment:
– AEPs educate clients about proper exercise techniques, injury prevention strategies, and the importance of gradual progression to avoid overuse injuries.
– By empowering clients with knowledge and skills, AEPs enable them to make informed decisions about their exercise routines and reduce the likelihood of injury.
5. Monitoring and Progression:
– AEPs monitor clients’ progress regularly, adjusting exercise programs as needed to ensure continued improvement and injury prevention.
– By tracking performance metrics and functional outcomes, AEPs can identify potential red flags and intervene proactively to mitigate injury risk.
6. Collaboration with Healthcare Professionals:
– AEPs work collaboratively with other healthcare professionals, such as physiotherapists, sports medicine physicians, and allied health practitioners, to provide comprehensive care for clients with complex needs or medical conditions.
– By coordinating care and sharing information, AEPs ensure that clients receive integrated support for injury prevention and management.
Overall, accredited exercise physiologists play a vital role in preventing future injuries by designing individualized exercise programs, addressing movement dysfunctions, and empowering clients with knowledge and skills to maintain their physical health and well-being.

Adaptive Fitness for Injury or Long-term Disability
Adaptive fitness opens doors to physical activity and well-being for individuals facing mobility challenges. It emphasizes inclusive exercise options tailored to different abilities, promoting not only physical health but also enhancing overall quality of life through active engagement. Complete cessation of activity with onset of injury or disease can often greatly hinder the individual’s mental and physical health.

Inclusive Workout Routines
Adaptive exercises are tailored to accommodate various disabilities, ensuring everyone can participate in fitness routines that suit their needs:
– Working around injury: Individuals with recent acute injury are still encouraged to keep exercising if advised by a health professional. Completing exercises that don’t use the injured part of the body, or finding ways to work within a limited range can be ideal whilst waiting for an injury to heal.
– Mobility Impairments: Modified exercises focusing on seated workouts, using weights and resistance in different ways for strength training, and wheelchair-specific routines.
– Visual or Hearing Impairments: Techniques integrating tactile cues, visual prompts, or auditory aids for guidance during exercises.
– Cognitive Disabilities: Structured routines with simplified instructions and repetitive motions for improved coordination and cognitive engagement.

Incorporating Accessible Equipment and Facilities
Creating inclusive environments involves utilizing accessible equipment and facilities:
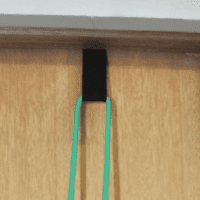
– Adaptive Equipment: Introduction to Velcro straps/cable fittings, specialized gear like hand cycles, adaptive rowing machines, and inclusive weightlifting apparatus.
– Accessibility Tips: Guidance on choosing fitness centers equipped with ramps, wider pathways, and adjustable machines to accommodate diverse needs.
– DIY Adaptations: Innovative adaptations for common exercises using household items or basic tools, empowering individuals to exercise independently at home.
Maintaining an active lifestyle despite significant changes in physical capacity is achievable through the expertise of Accredited Exercise Physiologists. These professionals possess specialized knowledge in adapting exercise programs to accommodate injuries and illnesses, ensuring safe and effective physical activity tailored to individual needs. Unlike discouraging exercise, they emphasize finding appropriate ways to remain active, promoting both recovery and overall health. Taking the initiative to consult with an exercise professional today can mark the beginning of a proactive approach to recovery and lifelong well-being.
Exercise Physiologist Role
An accredited exercise physiologist plays a crucial role in adaptive fitness by designing and implementing exercise programs tailored to individuals with specific needs or disabilities. Here are some key aspects of their role:
1. Assessment: They assess the individual’s physical capabilities, medical history, and specific adaptive needs. This helps them understand the client’s limitations and abilities.
2. Program Design: Based on the assessment, they create personalized exercise programs that consider the individual’s abilities, goals, and any medical considerations. These programs are designed to improve strength, flexibility, cardiovascular fitness, and overall functional capacity.
3. Exercise Prescription: They prescribe specific exercises and activities that are safe and effective for the client’s condition or disability. This may include adaptive equipment or modifications to traditional exercises to accommodate limitations.
4. Monitoring and Progression: They monitor the client’s progress closely, adjusting the exercise program as needed to ensure continued improvement and safety. Progression may involve increasing intensity, duration, or complexity of exercises as the client improves.
5. Education and Support: They educate clients on proper exercise techniques, safety precautions, and the benefits of physical activity. They also provide motivational support to help clients adhere to their exercise programs.
6. Collaboration: They often work closely with other healthcare professionals, such as physical therapists, occupational therapists, and physicians, to ensure a comprehensive approach to the client’s health and well-being.
7. Advocacy and Empowerment: They advocate for their clients’ needs and rights within the fitness and healthcare communities. They empower clients by promoting independence and self-management of their fitness goals.
Overall, accredited exercise physiologists play a vital role in adaptive fitness by promoting physical activity and improving quality of life for individuals with disabilities or specific health conditions through safe and effective exercise programs.