What is FHL Tendinopathy?
FHL tendinopathy refers to a condition where a person experiences pain due to damage or degeneration of the collagen fibres that make up the Flexor Hallucis Longus (FHL) tendon. This condition can occur in one of three locations along the FHL tendon: at the back of the ankle, under the mid-foot, or under the base of the big toe.
In contrast, swelling or inflammation in the sheath surrounding the FHL tendon marks the condition of FHL tenosynovitis. FHL tendinopathy and tenosynovitis often occur simultaneously, and people often use the terms interchangeably.
To summarise, FHL tendinopathy and FHL tenosynovitis are related conditions that cause pain and discomfort in the foot and ankle. The damage or degeneration of the collagen fibres of the FHL tendon causes FHL tendinopathy, while inflammation of the sheath surrounding the tendon causes FHL tenosynovitis.
What are Tendons?
Tendons are strong, fibrous connective tissues that attach muscles to bones. They are essential for movement and stability of the body. Although a tendon injury may seem to happen suddenly, it usually results from the accumulation of many tiny tears to the tendon over time.
Who Suffers from FHL Tendinopathy or Tenosynovitis?
FHL tendinopathy and tenosynovitis are most commonly seen in athletes and individuals who engage in repetitive or prolonged loading of the FHL tendon during their training or work. Some of the populations that are most susceptible to these conditions include:
- Athletes of all ages who participate in activities that require large amounts of forefoot push-off, such as running, jumping, hopping, and rising onto the toes. This includes ballet dancers, long-distance runners, football players, ice skaters, divers, and gymnasts.
- Individuals who have recently returned to physical activity involving large amounts of forefoot push-off.
- Workers in standing-based roles such as correctional or security officers, nurses, and hospitality staff.
What are the Signs and Symptoms of FHL Tendinopathy or Tenosynovitis?
The signs and symptoms of FHL tendinopathy or tenosynovitis typically develop gradually and are less likely to occur with acute trauma. Some common symptoms of FHL tendinopathy or tenosynovitis due to gradual onset include:
- Dull ache that worsens to sharp pain during forefoot push-off activities, such as walking, running, jumping, hopping, and rising onto the toes or demi-pointe and pointe work (in ballet dancers)
- Pain along the FHL tendon, which can occur in several locations, including the back or inside of the ankle, underneath the arch of the foot, and underneath the base of the big toe.
- Swelling in the back/inside of the ankle.
- Occasional clicking at the back or inside of the ankle.
- Pain with movement of the big toe.
- Potential locking or catching of the big toe if left untreated.
Acute cases of FHL tendinopathy or tenosynovitis are rare, but if they occur, the symptoms are similar to those of overuse-induced cases. However, the injury mechanism will be different, usually resulting from a direct, blunt knock to the back of the ankle.
(Brukner & Khan, 2006; Howell, 2015; Mak & Assai, 2016; Michelson & Dunn, 2005; Peters, 2015)
Why Does FHL Tendinopathy or Tenosynovitis Occur?
FHL tendinopathy or tenosynovitis usually occur due to repetitive or prolonged overloading of the FHL tendon. The FHL tendon is designed to assist with ankle, foot, and big toe movement, enabling activities like running, jumping, and rising onto the toes. However, when the FHL tendon is subjected to excessive, repetitive or prolonged loading, without sufficient time to adjust or heal, it can become overused. This overuse results in small tears to the collagen fibres that make up the tendon, ultimately leading to the tendon’s inability to function correctly, and causing pain and dysfunction.
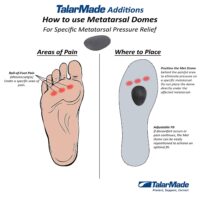
Other factors that may contribute to FHL tendinopathy or tenosynovitis include inadequate footwear, training errors, muscle imbalances, and decreased flexibility.
What are the Risk Factors for FHL Tendinopathy and or Tenosynovitis?
FHL tendinopathy and tenosynovitis can be influenced by various intrinsic and extrinsic factors, including:
Intrinsic Factors
- Poor foot and ankle control
- Weak or tight muscles in the foot and leg
- Incorrect training technique
- Previous injury
Extrinsic Factors
- Training activities that involve forefoot push-off, such as running, jumping, and dancing
- Recent changes in training program or intensity
- Training environment, such as surface and footwear
- Amount of training and frequency of training sessions
- Inadequate warm-up and cool-down routines
- Fatigue from overtraining or lack of rest periods.
Other factors such as age, gender, and genetics may also contribute to the development of FHL tendinopathy and tenosynovitis.
How is FHL Tendinopathy or Tenosynovitis Diagnosed?
FHL tendinopathy and tenosynovitis can be accurately diagnosed using several methods. Your physiotherapist will usually start by asking you questions about your injury, followed by conducting a physical examination.
The physical examination will involve looking for specific symptoms, such as pain with palpation, swelling, and tenderness along the FHL tendon. Your healthcare provider will also perform functional tests to assess foot and ankle strength, range of motion, and gait analysis. They may also check for other contributing factors, such as poor foot mechanics or muscle imbalances.
Imaging, such as ultrasound or MRI, may also be used to assist in diagnosis. Ultrasound can identify inflammation, thickening, or tears within the tendon and surrounding tissue. MRI can provide more detailed information about the extent of the damage and the presence of any associated conditions such as bone marrow oedema or stress fractures. However, imaging is not always necessary for diagnosis and is typically reserved for cases where there is a suspected severe or chronic injury.
In summary, the diagnosis of FHL tendinopathy and tenosynovitis involves a combination of a thorough physical examination and possibly imaging tests, depending on the severity of the injury.
Treatment for FHL Tendinopathy and Tenosynovitis
Treatment for FHL tendinopathy and tenosynovitis includes a combination of strategies aimed at relieving pain, reducing inflammation, and promoting tendon healing. Here are some of the treatment options:
Exercise:
Exercise is crucial in managing FHL tendinopathy and tenosynovitis and facilitating the FHL tendon’s recovery. Your physiotherapist will develop an exercise programme tailored to your condition and recovery stage, focusing on load management, activity modification, and activity prioritisation to ensure that your training sessions and activities do not aggravate your pain.
Stretches, Massage, Foam Rollers, and Trigger Balls:
Stretches, massage, foam rollers, and trigger balls can be utilised to help lengthen tight muscles, decrease the tension on the FHL tendon, and promote healing.
Transverse Frictions and Ultrasound:
Transverse friction or tendon massage and ultrasound are techniques that can assist in healing FHL tendinopathy and tenosynovitis by increasing circulation to the affected area. These techniques are only used if they are well-tolerated by the individual.
Adjacent Joints and Lower Limb Biomechanics:
Your physiotherapist will also assess and address any biomechanical issues in the surrounding joints and muscles to prevent the FHL from overloading and overworking the FHL tendon.
Medications:
NSAIDs, corticosteroids, and other pain and anti-inflammatory medications can be used in conjunction with physiotherapy to manage pain and inflammation locally. A GP or sports doctor may need to prescribe these medications.
Splinting:
Splinting is generally only utilised in advanced cases, where the tendon constriction is severe and non-responsive to other conservative treatments.
Surgery:
Surgery is a last resort for advanced cases where conservative treatment strategies have failed. Physiotherapy is typically followed after surgery to help with rehabilitation and a safe return to regular activity.
How is Your Treatment Rehabilitation Monitored?
It’s important to monitor your progress throughout your rehabilitation program to ensure that you’re on track to a safe and successful recovery. Your physiotherapist will work with you to regularly assess your ability level by retesting some outcome measures. But monitoring your progress isn’t just the physiotherapist’s responsibility – you can take an active role too. Keep track of any changes in your symptoms, ask questions, and share any concerns with your physiotherapist.
Additionally, your support team (family, boss, coach, teachers, etc.) can play a crucial role in your recovery. Encourage them to work with your physiotherapist and provide any necessary accommodations to help you reach your treatment goals. Remember, your recovery is a team effort!
Related Articles
- Understanding Tendon Injuries: Prevention and Treatment – Readers will learn about general strategies for preventing and treating tendon injuries, applicable to FHL tendinopathy.
- Foot Pain: Causes, Symptoms, and Solutions – This article likely discusses various conditions that cause foot pain, including FHL tendinopathy, offering a broader understanding of foot health.
- The Role of Exercise in Managing Foot and Ankle Tendon Injuries – Insights into how exercise can aid in the recovery and management of tendon injuries, specifically relating to the foot and ankle, are provided here.
- Ankle Pain: Identifying and Treating Common Conditions – An overview of conditions that cause ankle tendon pain, possibly including FHL tendinopathy, helps readers identify their symptoms.
- Rehabilitation Exercises for Foot and Ankle Injuries – Detailed exercise programs designed to strengthen the foot and ankle could be crucial for individuals recovering from FHL tendinopathy.
- Overcoming Common Foot and Ankle Injuries in Athletes – Given that athletes are at high risk for FHL tendinopathy, this article might focus on prevention, diagnosis, and treatment strategies tailored to an athletic population.
- The Importance of Proper Warm-Up and Cool-Down Routines for Foot Health – Explaining how these routines can prevent foot and ankle tendon injuries, including FHL tendinopathy, would be beneficial for readers.
Common Foot Pain Causes


Various factors, ranging from injuries and tendon problems to degenerative conditions and systemic diseases, can cause foot pain. Some common causes of foot pain include foot injuries, plantar fasciitis, bunions, metatarsalgia, Morton's neuroma, tendon injuries, bone injuries, degenerative conditions like arthritis, biomechanical issues, nerve-related sources such as tarsal tunnel syndrome, and muscle injuries.
Certain systemic conditions like fibromyalgia, lupus, rheumatoid arthritis, and psoriatic arthritis can also contribute to foot pain. This comprehensive list covers a wide range of foot pain causes, encompassing different areas of the foot and various underlying conditions.
Foot Injuries
Tendon Injuries
- Achilles Tendon Rupture
- Achilles Tendinopathy
- FHL Tendinopathy
- Peroneal Tendinopathy
- Tibialis Posterior Tendinopathy
Bone Injuries
- Ankle Fracture (Broken Ankle)
- Stress Fracture
- Stress Fracture Feet
- Severs Disease
- Osteochondritis Dissecans
- Heel Spur
- Shin Splints
Traumatic Ankle Ligament Injuries
Degenerative Conditions
Soft Tissue Inflammation
Biomechanical Conditions
Nerve-Related Sources
Muscle Injuries
Systemic Conditions
Soft Tissue Inflammation
Other Useful Information
Foot, Ankle & Heel Pain FAQs
Introduction
Welcome to PhysioWorks' comprehensive FAQ page on Foot, Ankle, and Heel Pain. Our expert physiotherapists are here to guide you in managing and overcoming discomfort. We’ve organised the FAQs into categories, each with a brief overview and links to in-depth articles, making navigation and understanding easier for you.


Foot Pain
Step into the various causes of foot pain and learn effective ways to relieve discomfort. Understand the impact of activities like barefoot running.
Ankle Injuries
Explore common ankle injuries and how to address them. From sprains to ligament damage, find out the best practices for care and prevention.
Heel Pain
Uncover the reasons behind heel pain and the effective treatments available. This section is particularly useful for understanding conditions like plantar fasciitis and heel spurs.
Achilles Pain
Find out how to manage and treat Achilles tendinopathy, a common concern for athletes and active individuals.
Shin Pain
Learn about shin splints, their causes, and how to alleviate this common issue, especially among runners.
Youth Injuries
Gain insights into youth leg injuries, including growing pains and heel issues in children.
Balance & Proprioception
Enhance your balance and proprioception with our professional advice and exercises.
Related Articles
- Sprained Ankle Treatment & Recovery Guide: Offers detailed advice on how to manage sprained ankles, including immediate recovery steps and physiotherapy treatments.
- Ankle Pain: Effective Management And Treatment Options: Discusses various conditions leading to ankle pain and outlines effective treatment strategies, highlighting the role of physiotherapy in pain reduction and mobility improvement.
- Plantar Fasciitis: Provides an overview of plantar fasciitis, including common causes, treatment options, and related conditions like peroneal tendinopathy and Achilles tendinopathy.
- Achilles Tendinopathy: Focuses on the causes of Achilles tendinopathy, its impact on heel pain, and a range of treatment and prevention strategies.
- Ankle Strapping: Complete Guide To Injury Prevention: Explains the benefits of ankle strapping as a preventative measure against injuries, with a focus on techniques and materials.
- Heel Pain: Explores various causes of heel pain, including tendon injuries, foot injuries, bone injuries, and systemic conditions, alongside recommended treatments.