What is Plantar Fasciitis?
What is Plantar Fasciitis?
Plantar Fasciitis, a common source of heel pain, arises from inflammation or micro-tears in the plantar fascia. This band of tissue, crucial for foot mechanics, supports the arch and absorbs walking stresses. Causes range from repetitive foot strain to poor biomechanics.
Identifying the Causes
The primary culprits are traction and compression injuries. Traction injuries stretch the fascia excessively due to weak arch muscles or flawed foot mechanics. Compression injuries result from direct impacts, like stepping on hard objects, bruising the fascia.
Key Symptoms
Key signs include pain in the heel or arch, especially after rest or in the morning. As the condition worsens, this pain becomes more frequent and intense, indicating progression.
The Progression of Plantar Fasciitis
This condition evolves from occasional post-exercise pain to constant discomfort. Without intervention, it can lead to heel spurs, where calcium deposits form, complicating recovery.
Diagnosing Plantar Fasciitis
Diagnosis involves evaluating symptoms, history, and clinical examinations. Imaging techniques like X-rays or MRI may reveal fascia changes or heel spurs. Sometimes, additional tests are needed to exclude similar conditions.
Risk Factors
Factors increasing risk include:
- Intensive sports or jobs that stress the heel.
- Being overweight.
- Pregnancy-related ligament changes.
- Foot arch abnormalities.
- Age-related foot changes.
- Inappropriate footwear.
- Weak arch muscles.
- Certain medical conditions, like arthritis or diabetes.

Effective Treatment Strategies
Thankfully, about 90% of cases improve with early treatment. This may include physiotherapy, lifestyle changes, soft orthotics, and, occasionally, injections like corticosteroids for short-term relief.
The Role of Foot Biomechanics
Addressing foot biomechanics is crucial. Physiotherapists offer tailored treatments, including manual therapy, exercises, and sometimes orthotics. These interventions aim to correct underlying issues, preventing recurrence.
A Multistep Rehabilitation Approach
Effective rehabilitation covers multiple phases:
- Early Injury Protection
- Regaining Range of Motion
- Restoring Foot Arch Muscle Control
- Normalising Calf and Leg Muscle Control
- Correcting Foot Biomechanics
- Enhancing Running and Landing Techniques
- Gradual Return to Activities
- Footwear Assessment
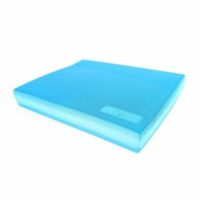
Exercises for Recovery
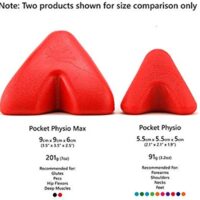
Focusing on strengthening foot muscles and loosening the calf is vital. Foam rollers are often chosen by the athletic population. Foot arch rollers seem to provide some people with temporary relief. Your physiotherapist will guide you through specific exercises tailored to your condition.
Exploring Other Treatment Options
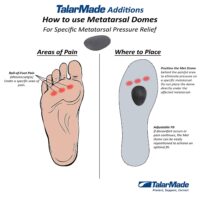
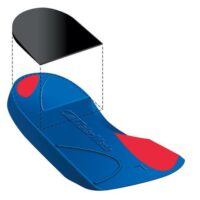
In cases of severe biomechanical issues, a combined approach of physiotherapy and podiatry is recommended. This may include taping, orthoses, and medication. Night splints and plantar fasciitis socks can provide additional support, but their long-term effectiveness varies. Some early research indicates that shockwave therapy may be helpful in recalcitrant cases, but the results do seem to vary.
The Impact of Weight and Load Management
Managing weight and foot load is essential, especially for individuals carrying extra weight, as it influences both the onset and duration of plantar fasciitis and heel spurs.
Conclusion: Seeking Professional Advice
Plantar fasciitis, while common, can significantly impact your daily life. Understanding its causes, symptoms, and treatment options is the first step towards recovery. However, every individual’s journey is unique.
Consulting a physiotherapist ensures you receive a personalised treatment plan, addressing not just the symptoms but also the root causes of your discomfort. Remember, early intervention is key to preventing long-term issues and getting back on your feet pain-free.
For specific guidance and a tailored treatment plan, please consult your trusted physiotherapist, doctor, or podiatrist.
Related Articles
- Heel Pain Causes and Treatment – Discover common causes of heel pain and various treatment options available.
- Foot Arch Pain Relief Strategies – Learn about what causes pain in the foot arch and how to alleviate it.
- Footwear and Orthotics for Plantar Fasciitis – Understand the importance of selecting the right footwear and how orthotics can help manage plantar fasciitis.
- Exercises for Strengthening the Foot Arch – Find out which exercises can strengthen the foot arch and potentially alleviate plantar fasciitis symptoms.
- The Role of Physiotherapy in Managing Heel Pain – Learn how physiotherapy can be used to treat heel pain, including plantar fasciitis.
- Plantar Fasciitis versus Heel Spurs – What’s the difference between the two conditions?
Common Foot Pain Causes


Various factors, ranging from injuries and tendon problems to degenerative conditions and systemic diseases, can cause foot pain. Some common causes of foot pain include foot injuries, plantar fasciitis, bunions, metatarsalgia, Morton's neuroma, tendon injuries, bone injuries, degenerative conditions like arthritis, biomechanical issues, nerve-related sources such as tarsal tunnel syndrome, and muscle injuries.
Certain systemic conditions like fibromyalgia, lupus, rheumatoid arthritis, and psoriatic arthritis can also contribute to foot pain. This comprehensive list covers a wide range of foot pain causes, encompassing different areas of the foot and various underlying conditions.
Foot Injuries
Tendon Injuries
- Achilles Tendon Rupture
- Achilles Tendinopathy
- FHL Tendinopathy
- Peroneal Tendinopathy
- Tibialis Posterior Tendinopathy
Bone Injuries
- Ankle Fracture (Broken Ankle)
- Stress Fracture
- Stress Fracture Feet
- Severs Disease
- Osteochondritis Dissecans
- Heel Spur
- Shin Splints
Traumatic Ankle Ligament Injuries
Degenerative Conditions
Soft Tissue Inflammation
Biomechanical Conditions
Nerve-Related Sources
Muscle Injuries
Systemic Conditions
Soft Tissue Inflammation
Other Useful Information
Foot, Ankle & Heel Pain FAQs
Introduction
Welcome to PhysioWorks' comprehensive FAQ page on Foot, Ankle, and Heel Pain. Our expert physiotherapists are here to guide you in managing and overcoming discomfort. We’ve organised the FAQs into categories, each with a brief overview and links to in-depth articles, making navigation and understanding easier for you.


Foot Pain
Step into the various causes of foot pain and learn effective ways to relieve discomfort. Understand the impact of activities like barefoot running.
Ankle Injuries
Explore common ankle injuries and how to address them. From sprains to ligament damage, find out the best practices for care and prevention.
Heel Pain
Uncover the reasons behind heel pain and the effective treatments available. This section is particularly useful for understanding conditions like plantar fasciitis and heel spurs.
Achilles Pain
Find out how to manage and treat Achilles tendinopathy, a common concern for athletes and active individuals.
Shin Pain
Learn about shin splints, their causes, and how to alleviate this common issue, especially among runners.
Youth Injuries
Gain insights into youth leg injuries, including growing pains and heel issues in children.
Balance & Proprioception
Enhance your balance and proprioception with our professional advice and exercises.
Related Articles
- Sprained Ankle Treatment & Recovery Guide: Offers detailed advice on how to manage sprained ankles, including immediate recovery steps and physiotherapy treatments.
- Ankle Pain: Effective Management And Treatment Options: Discusses various conditions leading to ankle pain and outlines effective treatment strategies, highlighting the role of physiotherapy in pain reduction and mobility improvement.
- Plantar Fasciitis: Provides an overview of plantar fasciitis, including common causes, treatment options, and related conditions like peroneal tendinopathy and Achilles tendinopathy.
- Achilles Tendinopathy: Focuses on the causes of Achilles tendinopathy, its impact on heel pain, and a range of treatment and prevention strategies.
- Ankle Strapping: Complete Guide To Injury Prevention: Explains the benefits of ankle strapping as a preventative measure against injuries, with a focus on techniques and materials.
- Heel Pain: Explores various causes of heel pain, including tendon injuries, foot injuries, bone injuries, and systemic conditions, alongside recommended treatments.