Metatarsalgia
Article by J.Miller, S.Armfield

Metatarsalgia: A Physiotherapist’s Guide
What is Metatarsalgia?
Metatarsalgia, commonly known as ball of foot pain, arises from issues with the metatarsals, the long bones in your foot. As physiotherapists, we see how this condition affects people’s daily activities and walking. Disrupting the balance of these bones can lead to mild to severe foot pain and potentially foot deformity.
Causes of Metatarsalgia
Multiple factors, including bone abnormalities and systemic diseases like diabetes, can cause metatarsalgia. The most frequent cause involves changes in the posture of the foot’s long bones. These bones bear your weight during walking, and any weakness, abnormal length, or stress fracture can disrupt their function.
Other causes include:
- Enlarged metatarsal head
- Arthritis or joint degenerative diseases
- Diabetes-related nerve pain
- Calluses or skin lesions disrupting weight distribution
- Age-related changes in footpad tissue
- High-impact sports
- Poorly fitting footwear
Symptoms to Watch Out For
The hallmark symptom of metatarsalgia is pain in the ball of the foot, especially noticeable when walking or engaging in sports. This chronic pain can hinder your ability to perform everyday tasks. Look out for discomfort in shoes and pain during activities that impact the feet, like running.
Metatarsalgia Treatment Approaches
Treatment varies depending on the cause. Here are some effective strategies:
- Footwear Adjustments: Choose shoes that evenly distribute weight across your foot. Avoid footwear that concentrates pressure on the ball and toes.
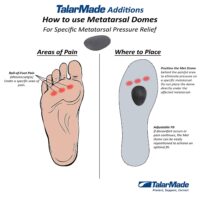
- Orthotics and Metatarsal Domes: These devices help separate foot bones, relieving pressure and preventing arch collapse. More info: Orthotics and Metatarsal Domes
- Massage: Massaging the affected area can ease swelling and pain, and improve circulation. More info: Foot massage.
- Anti-inflammatory Medications: While drugs like Ibuprofen may provide symptom relief, they do not tackle the underlying postural issues. Always consult a doctor before use.
- Targeted Exercises: PhysioWorks has developed foot arch posture exercises to strengthen foot muscles and correct foot posture. These can be more effective than passive solutions like orthotics.
The Importance of Foot Muscle Strength
Often, foot muscles weaken over time. The good news is that targeted exercises can often restore strength and function within weeks. However, it’s crucial to seek personalised advice from a physiotherapist, who can also identify other contributing factors like muscle tightness or referred pain.
When Surgery Might Be Necessary
In cases where non-invasive treatments fail, surgery might be an option.
Conclusion and Next Steps
Metatarsalgia can significantly impact your quality of life, but with the right approach, you can manage and alleviate the pain. Remember, footwear choices, orthotics, exercises, and professional advice play key roles in treatment. If you’re experiencing foot pain, don’t hesitate to consult a physiotherapist. We can provide tailored advice and treatment plans based on the latest research and your individual needs. Managing metatarsalgia effectively often means addressing the issue early, so seek professional advice to get back on your feet pain-free. Consult a physiotherapist or podiatrist for further advice on managing metatarsalgia.
Common Foot Pain Causes


Various factors, ranging from injuries and tendon problems to degenerative conditions and systemic diseases, can cause foot pain. Some common causes of foot pain include foot injuries, plantar fasciitis, bunions, metatarsalgia, Morton's neuroma, tendon injuries, bone injuries, degenerative conditions like arthritis, biomechanical issues, nerve-related sources such as tarsal tunnel syndrome, and muscle injuries.
Certain systemic conditions like fibromyalgia, lupus, rheumatoid arthritis, and psoriatic arthritis can also contribute to foot pain. This comprehensive list covers a wide range of foot pain causes, encompassing different areas of the foot and various underlying conditions.
Foot Injuries
Tendon Injuries
- Achilles Tendon Rupture
- Achilles Tendinopathy
- FHL Tendinopathy
- Peroneal Tendinopathy
- Tibialis Posterior Tendinopathy
Bone Injuries
- Ankle Fracture (Broken Ankle)
- Stress Fracture
- Stress Fracture Feet
- Severs Disease
- Osteochondritis Dissecans
- Heel Spur
- Shin Splints
Traumatic Ankle Ligament Injuries
Degenerative Conditions
Soft Tissue Inflammation
Biomechanical Conditions
Nerve-Related Sources
Muscle Injuries
Systemic Conditions
Soft Tissue Inflammation
Other Useful Information
Foot, Ankle & Heel Pain FAQs
Introduction
Welcome to PhysioWorks' comprehensive FAQ page on Foot, Ankle, and Heel Pain. Our expert physiotherapists are here to guide you in managing and overcoming discomfort. We’ve organised the FAQs into categories, each with a brief overview and links to in-depth articles, making navigation and understanding easier for you.


Foot Pain
Step into the various causes of foot pain and learn effective ways to relieve discomfort. Understand the impact of activities like barefoot running.
Ankle Injuries
Explore common ankle injuries and how to address them. From sprains to ligament damage, find out the best practices for care and prevention.
Heel Pain
Uncover the reasons behind heel pain and the effective treatments available. This section is particularly useful for understanding conditions like plantar fasciitis and heel spurs.
Achilles Pain
Find out how to manage and treat Achilles tendinopathy, a common concern for athletes and active individuals.
Shin Pain
Learn about shin splints, their causes, and how to alleviate this common issue, especially among runners.
Youth Injuries
Gain insights into youth leg injuries, including growing pains and heel issues in children.
Balance & Proprioception
Enhance your balance and proprioception with our professional advice and exercises.
Related Articles
- Sprained Ankle Treatment & Recovery Guide: Offers detailed advice on how to manage sprained ankles, including immediate recovery steps and physiotherapy treatments.
- Ankle Pain: Effective Management And Treatment Options: Discusses various conditions leading to ankle pain and outlines effective treatment strategies, highlighting the role of physiotherapy in pain reduction and mobility improvement.
- Plantar Fasciitis: Provides an overview of plantar fasciitis, including common causes, treatment options, and related conditions like peroneal tendinopathy and Achilles tendinopathy.
- Achilles Tendinopathy: Focuses on the causes of Achilles tendinopathy, its impact on heel pain, and a range of treatment and prevention strategies.
- Ankle Strapping: Complete Guide To Injury Prevention: Explains the benefits of ankle strapping as a preventative measure against injuries, with a focus on techniques and materials.
- Heel Pain: Explores various causes of heel pain, including tendon injuries, foot injuries, bone injuries, and systemic conditions, alongside recommended treatments.