Stress Fracture Feet
Article by Shane Armfield

What is a Foot Stress Fracture?
Stress fractures commonly occur in the foot, putting several bones at risk. Tiny cracks in a bone characterise a foot stress fracture. These cracks gradually develop over time and result in pain. The pain exhibits a distinct pattern, intensifying with increased engagement in weight-bearing activities like running or jumping.
What Causes a Stress Fracture?
Repeatedly applying force to an overloaded bone due to overuse, mainly through activities such as jumping or running long distances, leads to a stress fracture. While track and field athletes are especially prone to stress fractures, anyone can experience this condition. If you rapidly increase your weight-bearing exercise, you become more susceptible to developing a stress fracture. It can be a debilitating issue that hinders your ability to engage in any weight-bearing activity.
What is the Treatment for Stress Fractures in the Feet?
Phase I – Relieving Pain, Reducing Swelling, and Protecting the Injury
The primary objective of treatment for a stress fracture is pain relief. Your healthcare provider may prescribe analgesics to assist in managing the pain. Techniques such as ice therapy and unloading the inflamed structures are employed to minimise swelling and discomfort. Additionally, anti-inflammatory medications can be beneficial. Physiotherapists utilise various tools and methods, including ice, electrotherapy, acupuncture, deloading taping techniques, and soft tissue massage, to alleviate pain and reduce inflammation. In severe cases, the physiotherapist or doctor may recommend crutches or a walking boot.
Phase II – Restoring Normal Weight Bearing
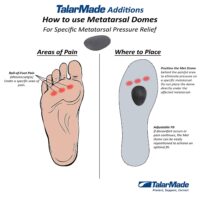
Careful management is crucial to avoid exacerbating the stress fracture by uncontrolled increases in weight-bearing. Once the pain and inflammation subside, the focus shifts to gradually reintroducing exercise. Treatment during this phase may involve massage, muscle and joint stretches, taping, or orthotics. Your physiotherapist will determine the most effective techniques for your specific needs.
Phase III – Restoring Normal Muscle Control and Strength
The proper functioning of your foot posture muscles plays a vital role in correcting biomechanical issues that contribute to increased stress on the foot. PhysioWorks has developed a “Foot Posture Correction Program” to restore your foot’s natural posture. Your physiotherapist will evaluate your foot posture muscles and prescribe targeted exercises tailored to your requirements. Consult your physiotherapist for personalised advice.
Phase IV: Restoring Full Function
This rehabilitation stage aims to help you regain your desired activity level. Specific treatment goals will vary depending on individual demands. For some, it may involve walking around the block. In contrast, others may aspire to run a marathon or engage in labour-intensive activities. Your physiotherapist will customise your rehabilitation program to help you achieve your functional goals.
Phase V: Preventing Recurrence
To prevent future stress fractures, your physiotherapist will educate you about gradually increasing exercise intensity. Consulting a dietitian for nutritional guidance during training can also be beneficial. Your physiotherapist will provide advice and support throughout this process.
Common Foot Pain Causes


Various factors, ranging from injuries and tendon problems to degenerative conditions and systemic diseases, can cause foot pain. Some common causes of foot pain include foot injuries, plantar fasciitis, bunions, metatarsalgia, Morton's neuroma, tendon injuries, bone injuries, degenerative conditions like arthritis, biomechanical issues, nerve-related sources such as tarsal tunnel syndrome, and muscle injuries.
Certain systemic conditions like fibromyalgia, lupus, rheumatoid arthritis, and psoriatic arthritis can also contribute to foot pain. This comprehensive list covers a wide range of foot pain causes, encompassing different areas of the foot and various underlying conditions.
Foot Injuries
Tendon Injuries
- Achilles Tendon Rupture
- Achilles Tendinopathy
- FHL Tendinopathy
- Peroneal Tendinopathy
- Tibialis Posterior Tendinopathy
Bone Injuries
- Ankle Fracture (Broken Ankle)
- Stress Fracture
- Stress Fracture Feet
- Severs Disease
- Osteochondritis Dissecans
- Heel Spur
- Shin Splints
Traumatic Ankle Ligament Injuries
Degenerative Conditions
Soft Tissue Inflammation
Biomechanical Conditions
Nerve-Related Sources
Muscle Injuries
Systemic Conditions
Soft Tissue Inflammation
Other Useful Information
Foot, Ankle & Heel Pain FAQs
Introduction
Welcome to PhysioWorks' comprehensive FAQ page on Foot, Ankle, and Heel Pain. Our expert physiotherapists are here to guide you in managing and overcoming discomfort. We’ve organised the FAQs into categories, each with a brief overview and links to in-depth articles, making navigation and understanding easier for you.


Foot Pain
Step into the various causes of foot pain and learn effective ways to relieve discomfort. Understand the impact of activities like barefoot running.
Ankle Injuries
Explore common ankle injuries and how to address them. From sprains to ligament damage, find out the best practices for care and prevention.
Heel Pain
Uncover the reasons behind heel pain and the effective treatments available. This section is particularly useful for understanding conditions like plantar fasciitis and heel spurs.
Achilles Pain
Find out how to manage and treat Achilles tendinopathy, a common concern for athletes and active individuals.
Shin Pain
Learn about shin splints, their causes, and how to alleviate this common issue, especially among runners.
Youth Injuries
Gain insights into youth leg injuries, including growing pains and heel issues in children.
Balance & Proprioception
Enhance your balance and proprioception with our professional advice and exercises.
Related Articles
- Sprained Ankle Treatment & Recovery Guide: Offers detailed advice on how to manage sprained ankles, including immediate recovery steps and physiotherapy treatments.
- Ankle Pain: Effective Management And Treatment Options: Discusses various conditions leading to ankle pain and outlines effective treatment strategies, highlighting the role of physiotherapy in pain reduction and mobility improvement.
- Plantar Fasciitis: Provides an overview of plantar fasciitis, including common causes, treatment options, and related conditions like peroneal tendinopathy and Achilles tendinopathy.
- Achilles Tendinopathy: Focuses on the causes of Achilles tendinopathy, its impact on heel pain, and a range of treatment and prevention strategies.
- Ankle Strapping: Complete Guide To Injury Prevention: Explains the benefits of ankle strapping as a preventative measure against injuries, with a focus on techniques and materials.
- Heel Pain: Explores various causes of heel pain, including tendon injuries, foot injuries, bone injuries, and systemic conditions, alongside recommended treatments.