Sinding Larsen Johansson Syndrome
Article by John Miller

What is Sinding Larsen Johansson Syndrome?
Sinding Larsen Johansson Syndrome is juvenile osteochondrosis that disturbs the patella tendon attachment to the inferior pole of the patella.
Sinding Larsen Johansson syndrome is an inflammation of the bone at the bottom of the patella (kneecap), where the tendon from the shin bone (tibia) attaches. It is an overuse knee injury rather than a traumatic injury.
What Causes Sinding Larsen Johansson Syndrome?
Sinding-Larsen-Johansson syndrome most likely results from a traction injury of the knee extensor mechanism at the junction of the patellar ligament and the inferior pole of the patella in the skeletally immature or adolescent athlete. This juvenile traction osteochondrosis is similar to Osgood-Schlatter syndrome.
Powerful repetitive quadriceps contractions cause a traction force on the inferior pole, disrupting the immature bone. There is a higher incidence in active exercising children during the adolescent growth spurt.
As a child grows, bones go through different stages of development.
- The patella pole is initially cartilaginous (cartilaginous stage).
- It then enters the apophyseal stage when the secondary ossification centre (apophysis) appears.
- The unity of the proximal tibial epiphysis with the tibial apophysis marks the epiphyseal stage.
- Lastly, when the growth plates fuse, the bony stage has been reached.
Children are most susceptible to Sinding-Larsen-Johansson syndrome when their bones are in the (2nd) apophyseal stage. During this phase, the apophysis is unable to withstand high tensile forces. When presented with robust and repetitive muscle contractions, micro-fractures occur in the immature area.
A potential cause of Sinding-Larsen-Johansson syndrome may be the lack of growth of the quadriceps compared to the femur. During a growth spurt in a child, the lengthening of the muscle is unable to keep up with the lengthening of the rapidly lengthening femur, resulting in an increased tensile force on the patella.
Sinding-Larsen-Johansson Syndrome is more likely in very active children who participate in sports that involve running, twisting, and jumping, such as basketball, football, volleyball, soccer, tennis, figure skating, and gymnastics.
What the Symptoms of Sinding Larsen Johansson Syndrome?
Localised pain, swelling or tenderness is felt at the front of your knee – at the base of your patella (kneecap), where the patella tendon inserts into the patella.
Patients are typically active boys aged 10 to 13 years but can also affect active girls a couple of years younger. Symptoms are usually:
- Worse with exercise, stair climbing, squatting, kneeling, jumping and running.
- Cause you to limp post-exercise (as the condition progresses)
- Unilateral or bilateral.
- Is relieved by rest
How is Sinding Larsen Johansson Syndrome Diagnosed?
Sinding Larsen Johansson Syndrome is typically diagnosed clinically by your physiotherapist or doctor. Knee X-ray may identify calcification or ossification at the patella – patella ligament junction. MRI scan will confirm and exclude other musculoskeletal injuries.
For an accurate diagnosis, please consult your knee physiotherapist or doctor.
Treatment for Sinding Larsen Johansson Syndrome
Physiotherapy assessment and treatment is a proven benefit for Sinding-Larsen-Johansson syndrome sufferers. Left untreated, most patients will fully resolve their symptoms within 3 to 18 months (Duri et al. 2002). With proper management, most athletes will return to their sport within 6 to 14 weeks (Iwamoto et al. 2009).
Phase 1 – Knee Load Management
- Immediate restriction of high impact activities, e.g. jumping and running.
- Low impact activities, e.g. cycling, cross-trainer, water running or swimming, are usually asymptomatic.
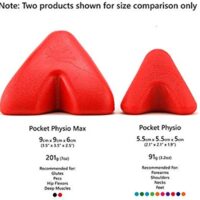
- Use an infrapatellar knee strap to dissipate forces away from the site of Sinding-Larsen-Johansson syndrome. (Duri et al., 2002) Here’s an example Sinding-Larsen-Johannesson brace.
- Kinesiology taping may provide both pain relief and load reduction at the site of pain and injury.
- Only on rare occasions, severe Sinding-Larsen-Johansson syndrome may require crutches.
Consult with your physiotherapist for the best advice specific to your knee.
Phase 2 – Anti-inflammatory Treatment
Ice & Electrotherapy
A combination of ice treatment, electrotherapy and a home tens unit will reduce pain and improve the healing rate. Ice usually eases the pain. Ice is useful at home or after exercise. (Michlovitz et al. 2007)
Phase 3 – Functional Training
Rest is also crucial in the management of Sinding-Larsen-Johansson syndrome and the relief of pain. It is best to discuss your exercise workload with your physiotherapist for advice on how to manage your return sport best while respecting your injury.
Whether or not you should continue playing sport is dependent on symptoms. Patients with mild symptoms may be able to continue to perform some or all sport. Others may choose to modify their program. In mild cases, it may enough to limit your physical activity so that the post-exercise pain is only slight and lasts for a maximum of 24-hrs. When symptoms become worse, it may be necessary to take a short break from your aggravating sports.
Phase 4 – Therapeutic Exercises
Stretching, Massage & Foam Rollers
One common reason for developing Sinding-Larsen-Johansson syndrome is excessively tight quadriceps muscles, ITB, hamstrings, hip flexors and calf muscles. (Iwamoto et al. 2009). Your physiotherapist will prescribe specific stretches for you if they assess that you are tight in these muscle groups.
Massage and foam rollers are beneficial, especially in the early phase when stretches create pain at the Sinding-Larsen-Johansson syndrome site.
Strengthening
Your muscle control around the knee will usually need attention to control or maintain your symptoms during the active phase of Sinding-Larsen-Johansson syndrome. Your physiotherapist will commonly prescribe or modify exercises for your quadriceps, hamstrings, calves, foot arch and gluteal (buttock) muscles. (Franchesci et al. 2007)
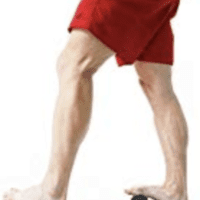
Foot Arch Control & Orthotics
Your foot biomechanics or arch control may be inadequate for your intensity of the sport. Your physiotherapist can assist both the assessment and corrective exercises for your dynamic foot control. Active Foot Correction Exercises can be beneficial as both a preventative and restorative strategy.
Occasionally, your foot biomechanics may be predisposing you to torsional stresses that can cause abnormal knee forces, which can cause knee injury. In these instances, foot orthotics may assist. There are mixed views on how effective these are since the foot structure is rapidly changing at this age. Ask your physiotherapist or podiatrist for advice.
The Prognosis for Sinding Larsen Johansson Syndrome
Sinding-Larsen-Johansson syndrome is a self-limiting syndrome. Complete recovery occurs with the closure of the patella growth plate. Although symptoms of Sinding-Larsen-Johansson syndrome may linger for months, few patients have poor outcomes with conservative treatment, and surgical intervention is seldom necessary.
For specific advice regarding your Sinding Larsen Johansson Syndrome, please seek the trusted advice of your knee physiotherapist or doctor.
Related Articles
- Kids Leg Pain: Understanding & Managing Youth Injuries – This article explores various leg injuries common among children, including Sinding Larsen Johansson Syndrome. Readers will find detailed explanations on symptoms, causes, and physiotherapy treatments.
- Osgood-Schlatter Disease – Offers insights into another condition that affects young athletes, similar to Sinding Larsen Johansson Syndrome, providing valuable information on symptoms, diagnosis, and treatment options.
- Patellofemoral Pain Syndrome (PFPS) – Discusses causes and treatments for knee pain arising from the patellofemoral region, which is relevant for understanding knee issues in adolescents.
- Quadriceps Tendinopathy – Focuses on injuries to the quadriceps tendon, explaining the healing process and rehabilitation strategies, which complements the information on Sinding Larsen Johansson Syndrome.
- Patellar Tendinopathy – Provides an overview of another common knee injury, detailing symptoms, causes, and treatment methods that could be beneficial for readers interested in knee health.
- Avulsion Fracture Recovery: A Physio’s Guide – Explains avulsion fractures, a type of injury related to the knee and other joints, covering recovery and physiotherapy approaches.