Greater Trochanteric Pain Syndrome (GTPS)
Article by Zoe Russell

Greater Trochanteric Pain Syndrome (GTPS)
Understanding and Managing Lateral Hip Pain
Introduction to Greater Trochanteric Pain Syndrome (GTPS)
Greater Trochanteric Pain Syndrome (GTPS) primarily affects the tendons and bursae near the greater trochanter, a prominent part of the femur on the hip’s side. This condition causes pain outside the buttock and thigh. GTPS includes gluteal tendon injuries and hip bursitis. The gluteus medius and minimus muscles’ tendons play a significant role in this syndrome. Tendinopathy, a result of excessive tendon load, is a common manifestation.
Common Causes of GTPS
GTPS can stem from direct trauma, prolonged hip pressure, repetitive movements like walking or running, inadequate exercise preparation, sustained weight-bearing on one leg, hip instability, or sporting injuries.
Identifying GTPS Symptoms
Symptoms include pain over the greater trochanter, possibly extending to the lateral thigh or leg. A notable ‘jump’ sign is evident when palpating the greater trochanter. Pain typically worsens over time and is exacerbated by sleeping on the affected side or weight-bearing activities.
Diagnosis Process
A physiotherapist or doctor will conduct an examination to distinguish GTPS from other conditions. Diagnostic imaging, like ultrasound or MRI, may be used for confirmation.
GTPS-Related Injuries
Consulting a physiotherapist is crucial for an accurate diagnosis.

Effective Treatment Strategies for GTPS
Treatment focuses on pain management, enhancing hip strength and control, and a gradual return to sports. Physiotherapy plays a pivotal role, divided into three phases:
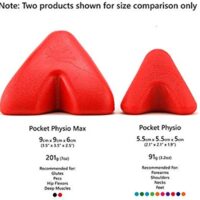
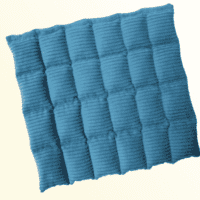
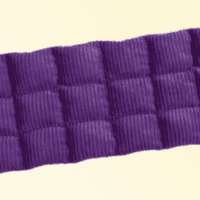
- PHASE I – Pain Relief & Protection: Managing pain through ice therapy, rest, and exercises. Techniques include ice, electrotherapy, acupuncture, taping, massage, and mobility aids.
- PHASE II – Restoring Normal Range of Motion (ROM) & Strength: After reducing pain and inflammation, the focus shifts to restoring hip joint ROM, muscle length, and tension. This phase includes strengthening, endurance, proprioception, balance exercises, and gait retraining, along with a tailored “Hip Core Stabilisation Program.”
- PHASE III – Restoring Full Function: Customised rehabilitation based on personal goals, focusing on a gradual return to desired activities. Ongoing hip stabilisation exercises are crucial to prevent recurrence.
Guidelines for Returning to Sport Post-GTPS
When returning to sport, it’s important to:
- Get clearance from your physiotherapist.
- Start below previous activity levels.
- Warm-up before exercise and apply ice afterward.
- Continue hip stabilisation exercises.
- Consult your physiotherapist if symptoms reappear.
Conclusion and Next Steps
GTPS, a condition impacting the hip’s tendons and bursae, requires a comprehensive treatment approach. A physiotherapist plays a critical role in diagnosing, treating, and guiding patients through recovery. Remember, patience is key in the healing process, and rushing can cause further damage. For personalised advice and effective management of lateral hip pain, it’s imperative to seek professional advice from a physiotherapist.
Recent Research Update:
New research emphasises the importance of individualised physiotherapy programs, particularly those focusing on strength and stability exercises for hip and core muscles, to effectively manage and prevent GTPS.
If you’re experiencing symptoms of GTPS or have concerns about hip pain, don’t hesitate to consult a physiotherapist for professional guidance and a tailored treatment plan.
Related Articles
- Trochanteric Bursitis – Hip Bursitis: Causes & Treatments: Offers insights into the causes and treatment options for hip bursitis, a condition closely related to GTPS.
- Gluteal Tendinopathy: Causes, Symptoms, And Treatment: Discusses the symptoms, causes, and treatment of gluteal tendinopathy, which is often associated with GTPS.
- Piriformis Syndrome – Understanding & Physio Treatment Tips: Provides information on managing Piriformis Syndrome, which can be relevant for those experiencing similar hip and buttock pain as seen in GTPS.
- Sacroiliac Joint Dysfunction (SIJ) Causes, Relief, Treatment: Explores SIJ dysfunction, offering additional context on lower back and hip pain that might be mistaken for or contribute to GTPS.
- Hip Flexor: Iliopsoas Groin Pain: Causes And Treatment: Covers causes and treatments for hip flexor and groin pain, which could be useful for readers seeking a broader understanding of hip-related issues.
Introduction to Hip & Groin Pain
Hip and groin pain affects a wide array of individuals, from athletes to the elderly. Understanding the common causes and treatments of this pain is vital for maintaining overall well-being and mobility.
Common Causes of Hip Pain
- Hip Joint Pain: This includes conditions like hip osteoarthritis, where the hip joint undergoes wear and tear, leading to inflammation and pain.
- Hip Labral Tear: A tear in the ring of cartilage surrounding the hip joint socket, often causing sharp pain during movement.
- Femoroacetabular Impingement (FAI): An abnormal hip joint shape that can lead to labral tears and arthritis.
- Stress Fracture: Small cracks in the hip bone, often due to overuse.
- Avascular Necrosis: Loss of blood flow to the femoral head, leading to joint destruction.
Lateral Hip Pain and Its Causes
- Greater Trochanteric Pain Syndrome: Inflammation of the tissues surrounding the hip.
- Gluteal Tendinopathy: Inflammation or irritation of the gluteal tendons.
- Trochanteric Bursitis: Inflammation of the bursa near the hip joint.
Groin Pain: Different Types and Causes
- Adductor-Related Groin Pain: Injuries to the muscles on the inner thigh.
- Osteitis Pubis: Inflammation of the pubic symphysis, often seen in athletes.
- Iliopsoas-Related Groin Pain: Strain or injury to the hip flexor muscles.
Other Muscle-Related Pain
- Piriformis Syndrome: Compression of the sciatic nerve by the piriformis muscle.
- Muscle Strain: Overstretching or tearing of muscle fibres.
- Core Stability Deficiency: Weakness in the core muscles, affecting hip stability.
Systemic Diseases Affecting the Hip
- Osteoporosis: Bone weakening, increasing fracture risk.
- Rheumatoid Arthritis: An autoimmune disease causing joint inflammation.
- Fibromyalgia: Widespread muscle pain and tenderness.
Referred Pain Sources
- Sciatica: Pain radiating along the sciatic nerve, which runs from the lower back through the hips and down the legs.
- Lower Back Pain: Can refer pain to the hip area.
- Pinched Nerve: Nerve compression in the spine or hip area.
Hip Surgery: A Solution for Severe Cases
- Hip Replacement: A surgical option for severe hip arthritis or damage.
What's New in Hip & Groin Pain Research?
Recent studies suggest the importance of tailored exercise programs in managing hip and groin pain. Physiotherapy techniques focusing on strengthening and stabilising the deep hip rotators and core muscles have shown significant improvements in pain management and mobility.
What to Do? Seeking Professional Advice
If you're experiencing hip or groin pain, it's crucial to consult with a physiotherapist or doctor.
They can assess your condition, provide a personalised treatment plan, and guide you through exercises tailored to your specific needs.
Conclusion
Hip and groin pain can significantly impact your quality of life. However, with the right knowledge and professional guidance, managing and overcoming this pain is achievable.
Related Articles
- Groin Pain Management - Expert advice on managing groin pain, covering causes such as adductor tendinopathy and femoroacetabular impingement.
- Hip, Groin & Buttock Pain FAQs: Symptoms, Causes, Treatments - Answers to frequently asked questions about hip, groin, and buttock pain, including symptoms, causes, and treatments.
- Hip Labral Tear - Information on hip labral tears, their symptoms, and treatment options.
- Piriformis Syndrome - Understanding & Physio Treatment Tips - Insight into piriformis syndrome, a condition causing buttock pain and how physiotherapy can help.
- Trochanteric Bursitis - Hip Bursitis: Causes & Treatments - An article explaining the causes of hip bursitis and offering treatment solutions.
- Groin Strain - Discusses groin strains, their symptoms, causes, and treatment methods.
- Gluteal Tendinopathy: Causes, Symptoms, And Treatment - Offers insights into the causes and treatment of gluteal tendinopathy.
Hip, Groin, Buttock Pain FAQs
Welcome to our comprehensive FAQ section, designed to address your concerns about hip, groin, and buttock pain. Here, we aim to provide clear, accessible information to help you understand the potential causes of your discomfort and the various treatment options available. Our physiotherapy experts have compiled a series of questions and answers to guide you through common issues, from hip impingement to sciatica, and everything in between. For more in-depth exploration, we've linked to related articles on our website, allowing you to delve deeper into each topic.


Hip Pain FAQs
Dealing with hip pain can be challenging, impacting your mobility and quality of life. Explore our detailed articles for insights on diagnosis, treatment options, and the importance of hip core muscles in maintaining joint health.
Lateral Hip Pain FAQs
Lateral hip pain, including conditions like gluteal tendinopathy and hip bursitis, requires targeted treatment strategies. Discover effective physiotherapy approaches to manage and alleviate your pain.
Groin Pain FAQs
Groin pain can significantly affect your ability to perform daily activities. Learn how to recognise serious symptoms and find effective relief methods through our expert advice.
Buttock Pain FAQs
Buttock pain, including conditions like SIJ pain and sciatica, can be debilitating. Our articles offer insights into symptoms, causes, and comprehensive treatment options to help you recover.
Conclusion
Our FAQ section is designed to be your go-to resource for hip, groin, and buttock pain. Whether you're dealing with a temporary discomfort or a chronic condition, understanding your symptoms and knowing the best treatment options is crucial. Remember, while our website provides valuable information, consulting a physiotherapist for a tailored diagnosis and treatment plan is always recommended. Explore our related articles for more in-depth knowledge and take the first step towards a pain-free life today.
Related Articles
- Greater Trochanteric Pain Syndrome (GTPS) - Readers can learn about the causes and management of pain near the greater trochanter, which is closely related to lateral hip pain.
- Trochanteric Bursitis - Hip Bursitis: Causes & Treatments - This article explains the causes of hip bursitis and offers treatment solutions, relevant to those experiencing lateral hip pain.
- Gluteal Tendinopathy: Causes, Symptoms, And Treatment - Offers insights into the causes and treatment of hip tendinitis, a condition linked to lateral hip pain.
- Hip Adductor Tendinopathy - Effective Physio Solutions - Focuses on groin pain caused by inflammation or degeneration of tendons in the hip region, directly relevant to the groin pain FAQ.
- Hip Flexor: Iliopsoas Groin Pain: Causes And Treatment - Provides detailed information on hip flexor issues, which can cause groin pain, making it highly relevant to readers of the original article.
- Hip & Groin Pain Guide: Causes, Treatment, Physio Advice - A comprehensive guide on hip and groin pain, covering common causes and treatments that align with the article's topics.
- Piriformis Syndrome - Understanding & Physio Treatment Tips - Discusses piriformis syndrome, a condition causing buttock pain, which is directly related to one of the SEO keywords.
- What Is Hip Impingement? - Explains hip impingement, a condition causing hip and sometimes groin pain, providing valuable insights into potential causes of the reader's discomfort.
- Sacroiliac Joint Dysfunction (SIJ) Causes, Relief, Treatment - Relevant for readers experiencing buttock pain, as it covers SIJ pain, a topic mentioned in the original article.
- Hip Arthritis - While not directly mentioned in the FAQ sections, hip arthritis can be a source of hip pain, making this article useful for readers wanting to understand more about hip conditions and pain management.