What is Compartment Syndrome?
Compartment syndrome, also known as recurrent or chronic exertional compartment syndrome (CECS), is a condition that affects the lower leg. Your lower leg is divided into four or five compartments with different muscles, nerves, blood vessels and tendons running through these compartments.
The compartment is surrounded by fascia, which helps to improve the efficiency of contraction and divide the muscle from surrounding tissue. Sometimes the pressure within one or more of these compartments increases to the point that the muscle, blood vessel or nerves are compressed. This can cause pain and loss of function. It is often found in runners as a result of the high repetitive loads that occur with running.
What Causes Compartment Syndrome?
Compartment syndrome can become evident with an increase in activity or training. As we use our muscles, there is a build-up of waste products and an increase in blood flow to the muscle. This causes the muscle volume to increase by between 8-20%, which results in increased pressure within the muscle compartment. There may also be an increase in the resting size of the muscle as a result of training. These changes are normal, with increased pressures reducing within 5 minutes of ceasing exercise.
Compartment syndrome seems to develop as a result of different anatomy.
- In some people, there is an extra ‘fifth’ compartment deep in the lower leg, with an extra sheath of fascia extending up the leg. The further the sheath extends, the greater the risk of compartment syndrome.
- The fascia becomes fibrotic or thickened as a result of a chronic inflammatory process or surgery. This leads to the fascia becoming less flexible.
In either case, pressure increases to a greater degree and takes longer to reduce post-exercise. The extra internal pressure in the compartment means reduced blood flow to the muscle and reduced oxygen for the muscle tissue. We think that the pain is due to a lack of oxygen supply. This is called ischaemic pain.
What are the Symptoms of Compartment Syndrome?
Tightness, burning, pressure, cramping and/or pain in the lower leg every time you exercise, most commonly around the calf and shin region. The pain commonly occurs in both legs.
The onset of these symptoms occurs at predictable intervals (for instance, 4 minutes into every run). Depending on which compartments are affected, you may also experience sudden fatigue on the top of your foot or ankle, numbness in the webbing near your big toe, or even drop your foot (this is quite uncommon). Sometimes there may be lumps or bumps in the tissue due to small hernias.
How is Compartment Syndrome Diagnosed?
It can be difficult to diagnose compartment syndrome as the pain in your leg could be caused by several other problems such as tendonitis, stress fracture or a condition called periostitis. Exertional compartment syndrome is usually diagnosed clinically by what causes the pain and its predictable nature. You have no pain at rest, but when you exercise, the pain comes on, which usually happens after a set period of time. If you continue to exercise, the pain gets worse but is usually completely relieved with rest.
Compartment syndrome can also be diagnosed with a needle inserted into the compartment attached to a pressure monitor. If the difference between the resting pressure and the pressure measured immediately after exercise is too high, this is a positive test for exertional compartment syndrome.
Compartment Syndrome Treatment
PHASE I – Pain Relief. Minimise Swelling & Injury Protection
Managing your pain. Pain is the main reason that you seek treatment. In truth, it was actually the final symptom that you developed and should be the first symptom to improve.
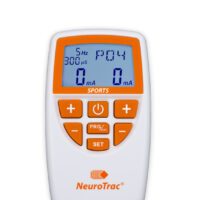
Your physiotherapist will use an array of treatment tools to reduce your pain and any chronic inflammatory disorder. These may include ice, electrotherapy, acupuncture, de-loading taping techniques, soft tissue massage, and temporary mobility aid (e.g. orthotics) to off-load the injured structures. They will advise you on any necessary modification of training or complete rest in severe cases.
PHASE II – Restoring Normal ROM & Posture
There is often a biomechanical fault leading to the increased load. Your physiotherapist will look to restore your normal joint range of motion, muscle length, neural tissue mobility, resting muscle tension, and fascial tissue flexibility.
Treatment may include joint mobilisation and alignment techniques, massage, muscle stretches and neurodynamic exercises, plus acupuncture, trigger point therapy or dry needling. Your physiotherapist is an expert in the techniques that will work best for you.
PHASE III – Restore Normal Muscle Control & Strength
Researchers have found different muscle firing patterns in runners with exercise-related leg pain. Your physiotherapist will assess your muscle recruitment pattern and prescribe the best exercises specific to your needs.
PhysioWorks has developed a “Foot Stability Program” to assist their patients in regaining normal muscle control. Please ask your physio for their advice.
PHASE IV – Restoring Full Function
This stage of your rehabilitation is aimed at returning you to your desired activities. Everyone has different demands for their bodies that will determine what specific treatment goals you need to achieve. For some, it is simply to run around the block. Others may wish to run a marathon.
Your physiotherapist will tailor your rehabilitation to help you achieve your own functional goals.
PHASE V – Preventing a Recurrence
Injuries and the pain associated does tend to return. Insufficient rehabilitation is thought to be one reason for this.
In addition to your muscle control, your physiotherapist will assess your biomechanics and start correcting any defects. It may be as simple as providing you with some foot orthotics to address any biomechanical faults in the legs or feet. Your physiotherapist will guide you on this.
What Results Can You Expect?
The advice that your physiotherapist gives you in conjunction with some ‘hands-on’ therapy can work to reduce your symptoms very well. Unfortunately, many people do not respond as well as we would like, usually due to their underlying anatomy. If we do not see the desired improvements, you may be referred to a sports doctor, podiatrist or orthopaedic surgeon.
Surgery
The surgery involves cutting the fascia that surrounds the muscle to allow for muscle volume increase. In some cases, surgical release is essential and urgent! Surgery is only considered if a conservative programme has failed and you want to keep exercising.
Other Treatment Options
Specific Interventions, e.g. Injection
Cortisone and other injected substances are usually not successful and are not recommended.
Massage
Many patients find that soft tissue massage therapy is beneficial to assist your pain relief, muscle relaxation and swelling reduction. Please ask your physiotherapist if you would benefit from massage.
Acupuncture
Acupuncture can be helpful for the relief of your pain. If you are interested in trying some acupuncture, many of our therapists are trained in acupuncture. Please ask for their advice.
Weight-Loss
Carrying excessive body weight can predispose you to injury or pain.
Article by John Miller
Calf Pain: Common Causes, Treatments and Solutions
Your Guide to Managing Calf Pain Effectively
Suffering from calf pain can throw a wrench in your daily routine, whether you're hitting the gym or just keeping up with your active lifestyle. Understanding the root causes of calf pain is essential for effective management and prevention. Let's dive into the common culprits of calf discomfort and how you can address them, guided by advice from physiotherapists.Calf Strains and How to Handle Them
Calf strains frequently occur among the physically active, marked by a sudden sharp pain or discomfort during movement. Adopting the RICE method—rest, ice, compression, and elevation—plays a pivotal role in treatment. More info: Strained Calf MuscleFacing Compartment Syndrome
Compartment syndrome is a serious condition where muscle pressure escalates to harmful levels, impeding blood flow and depriving muscle and nerve cells of necessary nutrients and oxygen. Prompt diagnosis is key to avoiding long-term damage. More info: Compartment SyndromeCombatting Cramps: Tips for Athletes
Muscle cramps often signal fatigue, dehydration, or electrolyte imbalance. Staying hydrated and maintaining a diet rich in essential nutrients can help prevent cramps, ensuring you stay on top of your game. More info: Muscle CrampsNavigating Achilles Injuries
Achilles injuries range from tendinopathy due to overuse to acute ruptures. These conditions require careful attention and, in the case of ruptures, immediate treatment to facilitate recovery and prevent further injury. More info: Achilles Tendinopathy

Incorporating New Research
Recent studies underscore the importance of targeted rehabilitation exercises and the potential benefits of other therapies in treating calf muscle pain. These advanced treatments can significantly improve outcomes, particularly for persistent cases. Please ask the advice of your physiotherapist or doctor on the nest treatment options or you.Dry Needling: A Game-Changer for Calf Muscle Pain
In recent years, dry needling has emerged as a revolutionary approach to alleviating muscle pain, offering a unique solution for those struggling with persistent calf discomfort. This technique involves inserting thin needles into specific points within the muscle, known as trigger points, to stimulate healing and relieve pain.Why Consider Dry Needling?
Physiotherapists recommend dry needling for several reasons:- Targeted Relief: By focusing on trigger points, dry needling works directly on the source of pain, providing rapid relief.
- Enhanced Recovery: This method not only reduces pain but also improves flexibility and increases blood flow, speeding up the recovery process.
- Complements Other Treatments: Dry needling can be used in conjunction with other physiotherapy treatments, such as manual therapy and exercises, to enhance overall effectiveness.
Is Dry Needling Right for You?
While dry needling is safe and effective for many, it's essential to consult with a physiotherapist to determine if this treatment is suitable for your specific condition. Your physiotherapist will assess your calf pain, taking into account your medical history and treatment preferences, to recommend the best approach for you. More info: Dry NeedlingConclusion: Embracing Comprehensive Care for Calf Muscle Pain
Calf pain need not hold you back from enjoying an active, fulfilling life. By understanding the causes, exploring treatment options like dry needling, and seeking professional advice, you can take control of your pain and embark on a path to recovery. Remember, a tailored approach to treatment, combining traditional physiotherapy methods with innovative techniques like dry needling, often yields the best results.What to Do? When to Seek Professional Advice
Experiencing calf muscle pain? Don't let it sideline you. Consult with a skilled physiotherapist or doctor for personalised advice and treatment options. Remember, early intervention can prevent complications and get you back on your feet sooner.Related Articles
- Calf Pain - Discover how common activities like running can lead to calf pain and the steps you can take to prevent it.
- Calf Strain & Calf Tear: Physio Treatment, And Recovery - Learn about the treatment and recovery process for calf strains and tears, essential information for anyone physically active.
- Achilles Rupture: Causes, Treatment & Management Options - Get insights into the causes of Achilles ruptures and the treatment options available for recovery.
- Compartment Syndrome - Explore the critical condition of compartment syndrome, its effects on the muscles, and the importance of timely treatment.
- Achilles Tendinopathy - Understand the symptoms of Achilles tendinopathy and the steps towards recovery.
- Leg Pain - This article provides a broad overview of leg pain, including causes related to the calf, and treatment options.
- Calf Pain Relief Products: Relieve Calf Muscle Pain Effectively - Discover how the OPPO 1010 Shin Support can provide relief for shin and calf pain.
- Moon Boot For Effective Lower Leg Injury Recovery - Find out how a moon boot can aid recovery from lower leg injuries, including those affecting the calf.
- Retrocalcaneal Bursitis - Learn about the impact of retrocalcaneal bursitis on the calf and treatment options.