Calcaneal Spur (Heel Spur)
Article by John Miller

Understanding Calcaneal Spurs
What is a Heel Spur?
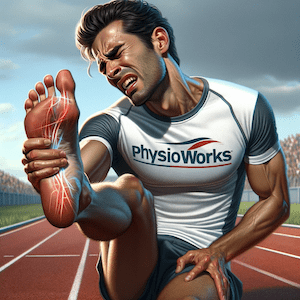
A calcaneal spur, commonly referred to as a heel spur, is a bone protrusion on the heel bone (calcaneus), which can extend into the arch of the foot, causing pain.
Origins of a Calcaneal Spur
The condition stems from the plantar fascia, a robust band of tissue aiding the arch of your foot. When it’s overstretched or suffers tears, plantar fasciitis can develop, often leading to a calcaneal spur due to persistent inflammation.
The Healing Process
If plantar fasciitis remains untreated, the body attempts to mend the weakened tissue by forming bone. Initially, fibroblasts repair the area, but if the injury lasts beyond six weeks, osteoblasts take over, leading to bone formation within the plantar fascia, resulting in a heel spur.
Recognising Symptoms
Early signs include pain under the heel after waking or resting, improving with activity but possibly presenting as a tender bump upon examination.
Diagnosing Calcaneal Spurs
Healthcare professionals diagnose calcaneal spurs by assessing symptoms, medical history, and conducting a physical exam. They also devise a treatment plan to prevent future occurrences.
Imaging tests like X-rays, ultrasounds, or MRIs can reveal a calcaneal spur. Additional tests might exclude other conditions.
Risk Factors
You’re more at risk of heel spurs if you’re active, overweight, pregnant, or spend much time on your feet. Foot structure issues, age-related changes, inadequate footwear, muscle weakness, arthritis, and diabetes are also risk factors.
Prognosis for Heel Spur Treatment
Most people with heel spurs see significant improvement with physiotherapy treatments. If non-invasive methods don’t yield results, corticosteroid injections might be an option, albeit with potential drawbacks for long-term healing.
Effective Treatment Approaches
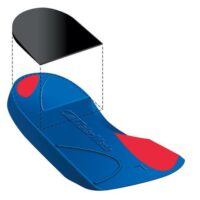
Addressing foot biomechanics is key. Treatments can include therapy, massages, stretching, plantar fascia bracing, foot strapping, arch strengthening exercises, and possibly custom orthotics prescribed by a podiatrist. Long-term stability may be enhanced with specific foot exercises.
Rehabilitation involves eight steps, focusing on pain relief, motion, muscle control, and correcting foot biomechanics, culminating in a return to activities with proper footwear.
Mechanical interventions, such as taping and using orthoses, can be more beneficial when paired with anti-inflammatory treatments. Night splints and weight control also contribute to managing calcaneal spurs.
Consequences of Inaction
Without treatment, calcaneal spurs can become larger and increasingly painful. It’s recommended to seek professional advice for a personalised approach to treating calcaneal spurs or plantar fasciitis. Please book your assessment to commence the best treatment for your calcaneal spur.
Related Articles
- Plantar Fasciitis – While not directly found in the initial search, this condition is closely related to calcaneal spurs, and an article on this topic would provide comprehensive care tips.
- Retrocalcaneal Bursitis – Offers insights into managing inflammation behind the heel bone, which can be relevant for readers experiencing heel pain.
- Achilles Tendinopathy – Explains the condition affecting the Achilles tendon, often associated with heel pain and relevant for understanding overall foot health.
- Foot Orthotics – Discusses how custom orthotics can help manage foot pain and support the arch, reducing the strain that contributes to calcaneal spurs.
- Stretching Exercises for the Foot and Heel – Provides readers with practical exercises to alleviate pain and improve flexibility, potentially slowing the progression of calcaneal spurs.
- Managing Acute Foot Injuries – This could guide readers on initial steps to take when experiencing foot pain, possibly preventing conditions like calcaneal spurs from worsening.
- Heel Pain in Children – If available, an article discussing common causes of heel pain in children, such as Sever’s disease, would complement the original article by covering a broader audience.
Common Heel Pain Causes
What's Causing Your Heel Pain?
This article digs into various heel pain and injury conditions that often trouble individuals. From the well-known discomfort of plantar fasciitis to the presence of heel spurs, we'll navigate through prevalent issues that impact our mobility.
Alongside discussions about frequently asked questions and recommended products, our exploration extends to traumatic ankle ligament injuries, tendon problems, foot injuries, bone fractures, degenerative conditions, biomechanical issues, nerve-related sources, muscle injuries, and systemic conditions. This comprehensive guide aims to provide clarity and understanding for those dealing with ankle and foot discomfort.


Heel Pain
FAQs & Products
Traumatic Ankle Ligament Injuries
Tendon Injuries
- Achilles Tendon Rupture
- Achilles Tendinopathy
- FHL Tendinopathy
- Peroneal Tendinopathy
- Tibialis Posterior Tendinopathy
Foot Injuries
Bone Injuries
- Ankle Fracture (Broken Ankle)
- Stress Fracture
- Stress Fracture Feet
- Severs Disease
- Heel Spur
- Shin Splints