Acute Soft Tissue Injury
Effective Management of Acute Soft Tissue Injuries
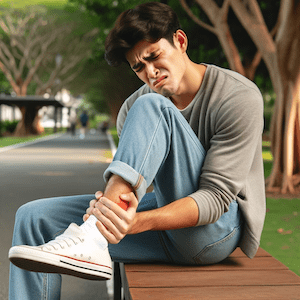
Acute soft tissue injury, including sprains and strains, are prevalent yet often not properly addressed. As physiotherapists, we witness the critical importance of swift and knowledgeable actions for a successful recovery. This article provides you with the essential knowledge and latest research-backed strategies to optimally manage these injuries.
What is the Acute Stage of a Soft Tissue Injury?
The acute soft tissue injury stage refers to the initial period following the injury, usually lasting from a few days up to a week, depending on the severity of the injury and the body’s response. During this phase, the body undergoes an inflammatory response, which is a natural part of the healing process. Here are the key characteristics and recommended actions during this stage:
Characteristics of the Acute Soft Tissue Injury Stage:
- Inflammation: Swelling, redness, and warmth in the affected area are common as blood flow increases to deliver healing cells and remove debris.
- Pain: The injury site is usually painful, especially when touched or moved. Pain serves as a protective mechanism to prevent further injury.
- Reduced Function: There may be a decrease in the range of motion or strength due to pain and swelling.
Seek Prompt Physiotherapy Advice
An early and precise evaluation can significantly influence your recovery path. Delaying assessment can obscure additional injuries such as minor fractures or dislocations. It’s crucial to consult a healthcare professional promptly after sustaining an injury. Minor injuries can have deeper impacts, highlighting the necessity of professional evaluation.
The Advantages of Immediate Care
Prompt treatment can lead to:
- Swift alleviation of pain
- Reduced reliance on painkillers
- Quicker resumption of daily activities
- Economic savings by reducing time off work
- Lower chance of injury recurrence
How Do You Treat an Acute Soft Tissue Injury?
Immediate self-care is vital:
- Rest actively, avoiding pain-triggering movements. Slowly reintroduce movement after the initial 48 hours to avoid complications.
- Apply ice initially to lessen swelling and pain. Switch to heat later to improve blood circulation and relax muscles.
- Use compression to limit swelling and support the injury, aiding the healing process.
- Elevate the injury above heart level when possible to reduce swelling.
What is the Fastest Way to Heal Soft Tissue?
Starting physiotherapy soon after injury can provide:
- Effective pain control
- Proper scar tissue formation guidance
- Speedier healing
- Customised rehabilitation exercises
- Enhanced function and prevention of future injuries
Recent research emphasises the benefits of early physiotherapy, highlighting quicker recovery and improved long-term function.
How Long Does it Take for Soft Tissue to Heal?
The healing time for soft tissue injuries can vary significantly based on the severity of the injury, the specific tissue damaged (muscles, tendons, or ligaments), and individual health factors including age, general health, and lifestyle choices such as smoking or having diabetes. Here’s a general guideline on the healing process and timelines:
Stages of Healing for Soft Tissue Injuries:
- Inflammatory Phase: This initial phase begins immediately after the injury and lasts up to 72 hours. The body initiates an inflammatory response to protect the area and start the healing process.
- Proliferative Phase: Lasting from about 2 days to 6 weeks, this phase involves the removal of debris, the growth of new blood vessels, and the production of scar tissue and collagen.
- Remodelling Phase: This final phase can last from 3 weeks to over a year. The body reorganises and strengthens the collagen fibres, improving the tissue’s strength and function.
What Part of the Body is Soft Tissue?
Soft tissue refers to the parts of the body that consist of muscles, tendons, ligaments, fascia, nerves, fibrous tissues, fat, blood vessels, and synovial membranes. These components play crucial roles in supporting, connecting, and surrounding other structures and organs within the body. Here’s a breakdown of each type of soft tissue:
- Muscles: Tissue that can contract to produce movement of the body parts.
- Tendons: Strong connective tissues that connect muscles to bones, allowing for the transmission of forces to create movement.
- Ligaments: Fibrous connective tissues that connect bones to other bones, providing joint stability.
- Fascia: Dense sheets of connective tissue that encase and connect muscles, organs, and other soft structures of the body.
- Nerves: Bundles of fibres that transmit electrical impulses throughout the body, responsible for sensing and responding to stimuli.
- Fibrous Tissues: Tissues that provide support and protection for the body’s structures, often found in tendons and ligaments.
- Fat (Adipose Tissue): Tissue composed of fat cells that store energy and provide insulation and protection.
- Blood Vessels: Arteries, veins, and capillaries that transport blood throughout the body, delivering oxygen and nutrients while removing waste products.
- Synovial Membranes: Specialised connective tissue that lines the inner surface of capsules of synovial joints and tendon sheath, producing synovial fluid for lubrication.
Soft tissues are found throughout the body and are essential for overall function, enabling movement, providing support, and protecting vital organs. They also play a key role in the body’s healing process and can be the source of pain and dysfunction when injured.

Latest Research and Techniques
Modern physiotherapy practices, including dry needling, advanced mobilisation techniques, and specific exercise programs, have shown promising outcomes in speeding up recovery and preventing future injuries.
Conclusion and Professional Advice
Effectively managing soft tissue injuries involves immediate medical advice, adequate self-care, and early physiotherapy. We advocate for a proactive approach to injury management. The right care at the right time can significantly enhance your recovery process and minimise the risk of long-term complications.
Seeking Professional Assistance: What to Do?
For sprains or strains, seeking professional advice is essential. A physiotherapist will offer a thorough assessment and a tailored treatment plan, crucial for optimal recovery and safe return to your usual activities. Your recovery journey begins with the step of professional care.
Related Articles
- Muscle Strain Treatment – Discover effective treatment options for muscle strains.
- Ligament Sprain Treatment – Discover effective treatment options for ligament sprains.
- Physiotherapy for Pain Relief – Learn how physiotherapy provides pain relief for various conditions, including soft tissue injuries.
- Injury Prevention Strategies – Gain insights into strategies to prevent common injuries, emphasising the importance of early intervention for soft tissue injuries.
- Rehabilitation Exercises for Soft Tissue Injuries – Explore customised rehabilitation exercises designed to aid the recovery of soft tissue injuries.
- Dry Needling for Muscle Recovery – Learn about modern techniques like dry needling for speeding up muscle recovery, relevant to the advanced practices mentioned.
Common Muscle Injuries
A Physiotherapist's Guide
Introduction
Muscle injuries, presenting as muscle strain, pain or myalgia, are prevalent health issues affecting a wide range of individuals. This detailed guide, from a physiotherapist's perspective, delves into various muscle injuries, elaborating on their management, prevention, and the importance of professional advice. Explore the linked articles for an in-depth understanding of muscle injuries and their effective treatment.
Neck & Back Muscle Injuries: Causes and Solutions
- Back Muscle Pain: This pain often results from prolonged poor posture or physical overuse. Key to relief is engaging in exercises that strengthen the core muscles and improve posture, thereby alleviating the strain on the back.
- Neck Sprain: Caused by sudden, awkward movements, a neck sprain can benefit from a combination of gentle stretches and targeted strengthening exercises to restore flexibility and strength.
- Text Neck: A modern ailment resulting from extended mobile device use, text neck can lead to chronic pain. Regular breaks, posture-awareness, and neck-strengthening exercises are essential for prevention.
- Whiplash: Commonly occurring in car accidents, whiplash requires a careful approach including neck stabilisation exercises and controlled movement to encourage healing and prevent further injury.
Lower Limb Muscle Injuries: Understanding and Treating
- Hamstring Strain: Particularly common among athletes, particularly runners, this strain demands rest initially, followed by a carefully structured rehabilitation program focusing on gradual strength building and flexibility.
- Thigh Strain: Often seen in sports involving sprinting and jumping, thigh strains need a combination of rest, ice, compression, and elevation (RICE) in the initial stages, followed by carefully planned strengthening exercises.
- Groin Strain: This injury requires a nuanced approach, including sufficient rest and targeted exercises, to ensure a safe and effective recovery.
- Calf Muscle Tear: Key to recovery is a balance of rest, gentle stretching exercises, and a gradual return to full activity, ensuring the muscle heals correctly and strength is regained.
Upper Limb Muscle Injuries: Prevention and Care
- Golfer's Elbow and Tennis Elbow: Both these conditions involve inflammation of the tendons and require a rest period, followed by ice therapy and specific exercises tailored to strengthen the affected muscles.
- Corked Thigh: Resulting from direct impacts, these injuries demand immediate application of ice and a controlled, gradual exercise regime for recovery.
- DOMS, Fatigue-Related Cramps & Myalgia: Adequate rest, good hydration, and gentle stretching are crucial in alleviating these conditions.
- RSI: Regular stretching, ergonomic workplace adjustments, and taking breaks are key preventive measures for repetitive strain injury.
Systemic Causes of Muscle Pain: A Holistic View
- Fibromyalgia: This complex condition demands a holistic treatment approach, including exercise routines, stress management techniques, and sometimes medication.
- Rheumatoid Arthritis: Effective management combines medication, gentle exercise, and regular physiotherapy sessions.
Prevention and Management Strategies
- Regular Exercise: Regular physical activity helps maintain muscle strength and flexibility, reducing the risk of muscle injuries.
- Posture Improvement: Good posture, both in motion and at rest, is crucial for preventing muscle strain.
- Proper Warm-up and Cool-down: Adequate warm-up before and cool-down after physical activity is vital in preventing muscle strains and injuries.
- Ergonomic Adjustments: Making ergonomic adjustments at work and during daily activities can significantly reduce the risk of repetitive strain injuries and other muscle-related issues.
- Maintaining a Healthy Weight: Keeping a healthy weight reduces the strain on muscles, particularly in weight-bearing joints.
What to Do? Seeking Professional Advice
Consult a physiotherapist or doctor for personalised advice and treatment plans. Remember, early intervention can significantly improve recovery outcomes and prevent chronic problems.
Conclusion
While muscle injuries are common, effective management and prevention are achievable with the right approach and knowledge. Understanding the causes, symptoms, and various treatments available empowers individuals to take proactive steps in their recovery and prevention. For the most tailored and effective treatment, always seek the guidance of a professional physiotherapist.
Common Ligament Injuries


Ligament Injury
Ligament injuries frequently occur in various body parts, leading to pain and restricted movement. The most common sites include the knee, ankle, shoulder, wrist, hand, and spine.
Notably, knee injuries like ACL, PCL, MCL, and LCL sprains are prevalent.
Shoulder injuries often involve the AC joint, while wrist and hand issues can include thumb and finger sprains.
Spinal ligament injuries, such as back and neck sprains, and whiplash, are also significant. Understanding these injuries helps in prevention, early detection, and effective treatment.
- Ankle Ligament Injuries
- Knee Ligament Injuries
- Shoulder Ligament Injuries
- Wrist & Hand Ligament Injuries
- Spinal Ligament Injuries
Ankle Ligament Injuries
Ankle injuries often result from sudden twists or rolls, leading to sprains and strains.
Knee Ligament Injuries
Knee ligament injuries are among the most common and can severely impact mobility and quality of life.
- ACL Injury
- PCL Injury
- MCL Sprain
- LCL Sprain
- Posterolateral Corner Injury
- Patella Dislocation
- Superior Tibiofibular Joint Sprain
Shoulder Ligament Injuries
Shoulder ligament injuries can be debilitating, affecting a range of movements.
Wrist & Hand Ligament Injuries
Injuries in the wrist and hand are common, especially in sports and physical activities.
Spinal Ligament Injuries
Spinal ligament injuries can result from various causes, including posture issues and physical impacts.
Related Articles
- Ligament Tear - Common Ligament Injuries: Offers a comprehensive overview of ligament injuries across different body parts, including prevention, early detection, and effective treatment strategies.
- Knee Ligament Injury - A Physiotherapist's Guide & Tips: Provides insights into diagnosing knee pain, covering ligament issues among other concerns, and suggests pain relief methods through exercise and treatment.
- Common Ankle Ligament Injuries: A Physiotherapist's Guide: Discusses the treatment and prevention strategies for ankle ligament injuries, emphasising the importance of early intervention.
- Sprained Ankle Treatment & Recovery Guide: Offers detailed guidance on the recovery timelines for sprained ankles, highlighting the importance of restoring strength, motion, and function for a full recovery.
- Ankle Strapping: Complete Guide To Injury Prevention: Focuses on preventing ankle injuries through effective strapping techniques and discusses conditions like ankle arthritis and biomechanical issues.
- Sub-Acute Soft Tissue Injury: Explores the treatment and recovery process for various ligament injuries, including those affecting the knee, shoulder, wrist, hand, and spine.
- Sprained Thumb Treatment And Recovery Tips: Delivers practical tips for treating and recovering from a sprained thumb, along with general management strategies for wrist and hand pain.
Common Tendinopathies
An Overview of Tendon Injuries
Tendinopathies affect individuals across various age groups and physical activities, and these prevalent musculoskeletal conditions cause pain and impaired function, significantly impacting the quality of life. Active individuals, including athletes and those engaged in repetitive occupational tasks, are particularly susceptible to these overuse injuries.
This article aims to provide a comprehensive overview of common tendinopathies, focusing on their specific manifestations and management approaches. By exploring the intricate details of conditions ranging from Achilles Tendinopathy to de Quervain's Tenosynovitis, we aim to enhance understanding and promote effective treatment strategies for those affected.
Tendinitis vs Tendinopathy
It's important to note that "tendinitis" is often used interchangeably with tendinopathy, but the suffix "-itis" implies inflammation, which is not always present in tendinopathies. In many cases, the condition involves degeneration of the tendon rather than acute inflammation. As a result, the more accurate term used nowadays is "tendinopathy."
Tendinopathy Treatments
Treatment approaches for tendinopathies typically focus on managing pain, promoting healing, and addressing contributing factors (e.g., overuse, improper biomechanics). Additionally, treatment approaches have advanced to include more targeted therapies, such as eccentric exercises, physiotherapy, and sometimes regenerative medicine techniques, depending on the specific type and severity of the tendinopathy.
Tendinopathy Classifications
Tendinopathy classifications have evolved to encompass a more nuanced understanding of these conditions. The modern tendinopathy classifications now include the following:
- Tendinitis or Tendonitis is an acute tendon inflammation, usually resulting from overuse, injury, or repetitive strain. It involves the active inflammatory process, and the symptoms can include pain, swelling, and limited range of motion.
- Tendinosis is a chronic degenerative condition of the tendon that occurs when repetitive micro-injuries do not have sufficient time to heal and repair properly. Unlike tendinitis, tendinosis does not primarily involve active inflammation. Instead, it is associated with a breakdown of collagen fibres within the tendon, leading to its structure and composition changes.
- Paratendonitis and Tenosynovitis: These conditions involve inflammation or irritation of the paratendon (the outer layer of the tendon) or the tenosynovium (the sheath surrounding certain tendons). Paratendonitis and tenosynovitis can lead to pain and limited function of the affected tendon and are often associated with repetitive motions or friction.
- Insertional Tendinopathy: This type of tendinopathy occurs at the point where the tendon attaches to the bone (the insertion site). It can involve inflammation, degeneration, or a combination of both at the tendon-bone interface.
- Mid-Substance Tendinopathy: Mid-substance tendinopathy refers to conditions affecting the central portion of the tendon rather than the attachment points. This tendinopathy is often related to chronic overuse and may involve changes in the tendon's structure without significant inflammation.
It's important to note that the classification and understanding of tendinopathies continue to evolve with ongoing research. If you suspect you have tendinopathy, it's best to seek evaluation and advice from a healthcare professional, such as your physiotherapist, who is experienced in tendon conditions.
Seeking Professional Advice
Consult a physiotherapist with a special interest in tendinopathies for personalised advice and treatment.
Specific Tendinopathies
Foot & Ankle
- Achilles Tendinopathy
- Achilles Tendon Rupture
- FHL Tendinopathy
- Peroneal Tendinopathy
- Tibialis Posterior Tendinopathy
Knee
Hip & Groin
Shoulder
Elbow
Wrist & Hand
Conclusion
Tendinopathy is a complex condition requiring careful diagnosis, treatment, and management. Understanding its phases, symptoms, and treatment options is vital for effective recovery.
What to Do?
If you suspect tendinopathy, consult a physiotherapist for a thorough assessment and tailored treatment plan. Remember, early intervention can significantly improve your prognosis and hasten recovery.
Related Articles
- Tendinopathy: Causes, Symptoms, And Effective Treatments - Discover a broad overview of tendinopathies, including causes, symptoms, and a variety of effective treatment options.
- Effective Tendinopathy Physiotherapy Treatment Strategies - Explore advanced physiotherapy treatment strategies for managing tendinopathies effectively.
- Biceps Tendinopathy: Causes, Symptoms, And Treatments - Gain insights into the specific causes, symptoms, and treatment options for biceps tendinopathy.
- Gluteal Tendinopathy: Causes, Symptoms, And Treatment - Learn about gluteal tendinopathy, its impact, causes, symptoms, and how it can be treated.
- Rotator Cuff Tendinopathy - Understand the specifics of rotator cuff tendinopathy, including its causes, symptoms, and various treatment methods.
- Proximal Hamstring Tendinopathy - Find detailed information on proximal hamstring tendinopathy, including prevention and treatment strategies.
- Peroneal Tendinopathy - We discuss the causes, symptoms, and rehabilitation processes for peroneal tendinopathy, and how to return to sports safely.
- Wrist Tendinopathy - Uncover the range of treatment options for wrist tendinopathy, from early injury treatment to physiotherapy modalities.
- Hip Adductor Tendinopathy - Effective Physio Solutions - Explore the causes, symptoms, and physiotherapy solutions for hip adductor tendinopathy.