SIJ & Buttock Pain Treatment Guidelines: Taking Action for Relief
When addressing SIJ and buttock pain, your physiotherapist aims to tailor your treatment according to your specific diagnosis. The treatment process can be broken down into different phases, each with its own objectives.
PHASE I - Relieving SIJ Pain & Protecting the Joint
Firstly, let's tackle pain relief. While acute SIJ dysfunction might lead to the prescription of pain relievers or anti-inflammatory meds, these won't address the root cause of SIJ pain. Instead, your healthcare practitioner, armed with an in-depth understanding of your SIJ's biomechanics and muscular control, will thoroughly evaluate chronic cases of SIJ dysfunction. Your priority is to manage sacroiliac pain, which typically drives individuals to seek treatment. In fact, it's often the final symptom to develop and should be the first to improve in most cases. Achieving natural short-term pain relief is possible through the use of ice or heat packs applied to your SIJ.
The next step involves managing inflammation. Ice therapy, exercises, and techniques to unload inflamed structures are effective methods. Non-steroidal anti-inflammatory drugs, like ibuprofen, might be recommended by your doctor. In certain cases, specialised blood tests can aid in diagnosing conditions like seronegative arthritis, which may predispose you to sacroiliitis. Addressing prolonged morning stiffness is crucial, especially in conditions like Ankylosing Spondylitis.
For SIJ instability, passive support can be beneficial, often through supportive taping. In cases of prolonged instability, a sacroiliac joint stabilisation belt might be suggested, although an exercise protocol tailored to your SIJ issue is generally more effective.
Remember, if you have questions, seek advice from your SIJ physiotherapist.
PHASE II - Restoring Normal Movement and Strength. Early Hip Core Exercises.
As your SIJ pain and inflammation subside, your focus shifts towards restoring your pelvic joint alignment and normalising dynamic muscle control affecting the SI Joints.
Your physiotherapist might start you on a core stability program for your lower abdominal muscles, crucial for stabilising your lower back and pelvis. A similar activation and strength program will target your deep gluteal muscles, often referred to as your hip core muscles. Your muscle recruitment pattern will be assessed to determine the most suitable exercises for your needs.
PHASE III - Regaining Full Function
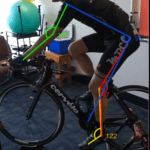
This phase concentrates on returning your normal pelvic alignment and maintaining sacroiliac joint range of motion during more demanding positions. Improving muscle power, proprioception, balance, and gait (walking pattern) are also key. Your physiotherapist tailors the treatment to fit your chosen sport or daily activities, ensuring a safe return to your desired level of function.
Keep in mind that different individuals have distinct demands for their sacroiliac joints, shaping their specific treatment goals. Whether it's a stroll around the block or running a marathon, your physiotherapist customises your sacroiliac joint rehabilitation to match your functional aspirations.
PHASE IV - Preventing Future Issues
Preventing the recurrence of sacroiliac joint dysfunction hinges on committing to a thorough muscle control program. A major contributing factor to its chronic nature is specific muscle weakness. Your physiotherapist will guide you in identifying the best exercises for you to continue regularly or intermittently.
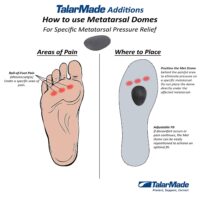
Beyond muscle control, your physiotherapist evaluates your SIJ, spine, hip, and lower limb biomechanics, addressing any shortcomings that might make you susceptible to SIJ pain and dysfunction. To fine-tune and maintain your sacroiliac joint stability and function, focus on rectifying deficiencies and learning self-management techniques. Your SIJ physiotherapist will provide professional guidance.
For more information, explore our detailed resources on SIJ Pain & Dysfunction.