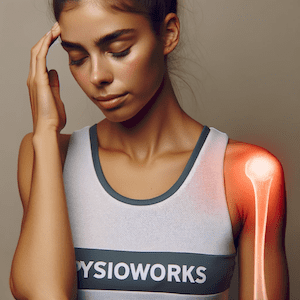
Shoulder Instability
Functional Shoulder Instability

Article by Harry Lawrence

What is Functional Shoulder Instability?
Functional Shoulder Instability occurs when the shoulder joint moves excessively, causing discomfort and a feeling of instability. This condition ranges from mild, unidirectional instability to multidirectional instability and recurrent shoulder dislocations.
Left untreated, it increases the risk of various injuries, including shoulder impingement, shoulder bursitis, rotator cuff tears, labral tears, and shoulder dislocations.
Causes of Functional Shoulder Instability
Functional shoulder instability results from neuromuscular imbalances rather than structural defects. It often stems from repetitive strain, muscular weakness, or insufficient neuromuscular control.
Common causes include:
- Overuse injuries
- Poor posture
- Muscle imbalances
- Inadequate proprioception
These factors affect the dynamic control of the shoulder joint. Moreover, sports involving repetitive overhead motions, such as swimming, tennis, throwing sports and volleyball, may contribute to the development of functional shoulder instability.
Symptoms
Symptoms of functional shoulder instability differ from those of structural instability. Patients frequently experience a sensation of the shoulder “giving way” or feeling unstable during specific movements, rather than full dislocations or subluxations. Recurrent episodes of pain, weakness, and a feeling of “looseness” during activities are also common complaints.
Diagnosis
Your physiotherapist will conduct a comprehensive assessment to diagnose functional shoulder instability. This includes taking a detailed history and performing a thorough physical examination, assessing range of motion, muscle strength, and stability.
While imaging like ultrasounds or MRI can identify underlying or secondary issues such as muscle tears or bony abnormalities, it cannot reveal functional instability.
Treatment Options
Effective management of functional shoulder instability typically involves a multifaceted approach tailored to your needs. Physiotherapy plays a central role in strengthening the muscles around the shoulder joint and improving proprioception.
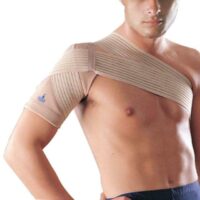
These exercises aim to enhance dynamic stability and correct muscular imbalances. Additionally, proprioceptive training, shoulder bracing, and activity modification strategies can help reduce symptoms and prevent further instability episodes.
Addressing contributing factors, such as poor posture and overuse injuries, is essential in preventing the recurrence of functional shoulder instability. Lifestyle modifications, including ergonomic adjustments and proper warm-up and cool-down routines, can significantly reduce symptoms.
What to Expect with Functional Shoulder Instability?
Rehabilitation time depends on your level of dysfunction. Those with mild, unidirectional instability and no prior history of shoulder problems recover more quickly than those with multidirectional instability, multiple dislocations, and concurrent shoulder blade dysfunction.
Improving shoulder strength and control is crucial for recovery. Your compliance with the exercise program significantly impacts your recovery time.
Will You Need Surgery?
Many individuals with functional shoulder instability respond well to conservative physiotherapy treatment. In severe cases, where conservative measures prove insufficient, surgical intervention may be considered as a last resort to restore stability and function to the shoulder joint. It may also be considered in cases with a secondary anatomical problem, such as a labral tear, significant rotator cuff tear, or Hill-Sachs lesion.
For more information, please do not hesitate to ask your shoulder physiotherapist.
Related Articles
- Effective Shoulder Impingement Treatment And Advice: Offers insights into shoulder impingement syndrome, a condition closely related to shoulder instability, where tendons are pinched during arm movements.
- Rotator Cuff Tear – Causes, Symptoms, Treatment: Discusses rotator cuff tears, which can be a consequence of or a contributing factor to shoulder instability.
- Strengthen Scapular Muscles: Enhance Your Shoulder Health: Highlights the importance of scapular stabilisation in improving shoulder health and preventing injuries, a key aspect of managing functional shoulder instability.
- Biceps Tendinopathy: Causes, Symptoms, And Treatments: Explores biceps tendinopathy, which can occur alongside shoulder instability due to similar risk factors like overuse and repetitive strain.
- Frozen Shoulder (Adhesive Capsulitis): Provides information on adhesive capsulitis or frozen shoulder, a condition that can emerge due to prolonged shoulder instability or immobility.
- Shoulder Pain: Offers a broad overview of common shoulder pain causes, including conditions related to shoulder instability.
Shoulder Pain Causes
Common Injuries & Conditions
Understanding the common shoulder pain causes is crucial, as this discomfort can stem from various issues like rotator cuff injuries, arthritis, and frozen shoulder. Our guide offers a comprehensive exploration of these causes, providing insights into both acute and chronic conditions. It aims to equip you with knowledge and strategies for effective treatment and recovery, catering to those grappling with recent injuries or long-term pain. This resource is your go-to for navigating the complexities of shoulder pain and its management.
Rotator Cuff
- Rotator Cuff Injury: A common condition causing shoulder pain, often due to repetitive overhead activities.
- Rotator Cuff Tendinopathy: Inflammation or damage to the rotator cuff tendons, leading to pain and reduced mobility.
- Rotator Cuff Calcific Tendinopathy: Characterised by calcium deposits in the rotator cuff tendons, causing intense pain.
- Rotator Cuff Tear: Involves a tear in the rotator cuff muscles, often resulting from injury or wear over time.
- Bicep Tendinopathy: Affects the bicep tendon, leading to pain in the front of the shoulder.
Shoulder Impingement Syndrome
- Shoulder Impingement: A condition where shoulder tendons are pinched during arm movements, causing pain and limited mobility.
- Shoulder Bursitis: Inflammation of the bursa, a small fluid-filled sac in the shoulder, causing pain and discomfort.
- Swimmer’s Shoulder: An overuse injury common in swimmers, causing shoulder pain and impingement symptoms.
Shoulder Stiffness
- Adhesive Capsulitis / Frozen Shoulder: A condition where the shoulder becomes stiff and painful, often developing gradually without a specific cause.
Shoulder Instability
- Shoulder Dislocation: Occurs when the shoulder joint is forced out of position, causing pain and instability.
- Functional Shoulder Instability: Chronic instability in the shoulder, often leading to recurrent subluxations, dislocations and pain.
Acromioclavicular Joint
- AC Joint Injury: Involves damage to the acromioclavicular joint, common in athletes and after falls.
Bone Conditions
- Shoulder Arthritis: Degenerative joint disease affecting the shoulder, causing pain and stiffness.
- Broken Shoulder / Fractured Humerus: A break in the shoulder bone, often resulting from trauma or falls.
- Stress Fracture: A small crack in the bone, typically caused by overuse and repetitive activities.
Post-Operative Physiotherapy
Post-Operative Shoulder Rehabilitation: Essential for recovery, involving tailored exercises and therapies to regain strength and mobility after shoulder surgery.
- Subacromial Decompression: A surgical procedure to alleviate shoulder impingement symptoms.
- Shoulder Arthroscopy: Minimally invasive surgery for various shoulder conditions.
- Acromioplasty: Surgery to reshape the acromion and relieve impingement.
- Rotator Cuff Repair: Surgical repair of a torn rotator cuff.
- SLAP Repair: Surgery to fix a specific type of labrum tear in the shoulder.
- Biceps Tenodesis: Surgical procedure to reattach the biceps tendon.
- Biceps Tenotomy: Involves cutting the biceps tendon to relieve pain.
- Total Shoulder Replacement: Replacement of the shoulder joint with artificial components.
Muscle Conditions
- Muscle Strain: A tear or stretch in a muscle, often causing pain and limited movement.
- DOMS – Delayed Onset Muscle Soreness: Muscle pain and stiffness that occurs hours after unfamiliar or strenuous exercise.
Neck Arm Syndromes
Referred Pain: Pain in the shoulder that originates from another area of the body, such as the neck or spine.
- Neck Arm Pain: Pain that originates in the neck and travels down to the arm and shoulder.
- Cervical Radiculopathy: Occurs when a nerve in the neck is compressed or irritated, leading to shoulder pain.
- Thoracic Outlet Syndrome: A condition where nerves or blood vessels between the collarbone and first rib are compressed, causing pain in the shoulder area.
Systemic Conditions
- Fibromyalgia: A chronic condition characterised by widespread musculoskeletal pain, including in the shoulder.
- Rheumatoid Arthritis: An autoimmune disorder that can cause joint pain and damage throughout the body, including the shoulders.
Shoulder Products & FAQs
Explore our range of shoulder products and find answers to frequently asked questions about shoulder pain and treatment options.
Shoulder Pain FAQs
Your Comprehensive Guide to Understanding and Managing Shoulder Injuries
Welcome to the "Shoulder Pain FAQs" page, your go-to resource for understanding various aspects of shoulder pain, injuries, and how to manage them effectively. The shoulder is a complex joint that allows for a wide range of movements, but it is also susceptible to various injuries and conditions that can cause discomfort and limitations in daily activities.
In this comprehensive guide, we will explore the most common shoulder injuries, their causes, and how to identify and treat them. We'll also address frequently asked questions about specific shoulder conditions, providing you with valuable insights into your shoulder health.
When Should You Worry About Shoulder Pain?
Shoulder pain can be caused by numerous factors, ranging from minor strains to more severe injuries. Knowing when to seek medical attention is crucial to prevent further damage and facilitate timely recovery.
Common Shoulder Injuries
We'll swing into the most prevalent shoulder injuries, shedding light on their causes, symptoms, and appropriate treatment options.
More info: Common Shoulder Injuries
What Causes Shoulder Pain?
Understanding the root causes of shoulder pain is fundamental to addressing the issue effectively. We'll explore the various factors that can lead to shoulder discomfort and how to mitigate them.
More info: What Causes Shoulder Pain?
What is Your Scapulohumeral Rhythm?
The scapulohumeral rhythm plays a vital role in shoulder function and movement. We'll explain what it is and its significance in maintaining a healthy shoulder.
More info: What is Your Scapulohumeral Rhythm?
Rotator Cuff: An In-Depth Analysis
The rotator cuff is a critical group of muscles and tendons in the shoulder. We'll dive into its anatomy, functions, and common problems associated with it.
More info: Rotator Cuff: An In-Depth Analysis
How Can You Tell If You Have Torn Your Rotator Cuff?
Identifying a torn rotator cuff can be challenging, but we'll provide you with essential signs to look out for and when to seek professional evaluation.
More info: How Can You Tell If You Have Torn Your Rotator Cuff?
Can You Diagnose A Torn Rotator Cuff Without An MRI?
Find out about diagnostic methods for a torn rotator cuff, including whether an MRI is always necessary for accurate diagnosis.
More info: Can You Diagnose A Torn Rotator Cuff Without An MRI?
Can You Lift Your Arm With A Rotator Cuff Tear?
Discover the limitations and challenges you may face if you have a torn rotator cuff and how to manage arm movement during the healing process.
More info: Can You Lift Your Arm With A Rotator Cuff Tear?
Will Your Shoulder Blade Hurt With A Torn Rotator Cuff?
Learn about the possible relationship between a torn rotator cuff and shoulder blade pain, and what it indicates about your shoulder health.
More info: Will Your Shoulder Blade Hurt With A Torn Rotator Cuff?
Will A Cortisone Injection Help A Torn Rotator Cuff?
Cortisone injections are sometimes used for shoulder pain, but their effectiveness in treating a torn rotator cuff is a point of interest we'll explore.
More info: Will A Cortisone Injection Help A Torn Rotator Cuff?
How Can You Make Your Rotator Cuff Heal Faster?
We'll provide practical tips and strategies to aid in the healing process of a torn rotator cuff and restore shoulder function more rapidly.
More info: How Can You Make Your Rotator Cuff Heal Faster?
Shoulder Bursitis: Understanding the Condition
What is shoulder bursitis, and how does it differ from other shoulder injuries? Get insights into this inflammatory condition and how to manage it.
More info: Shoulder Bursitis: Understanding the Condition
Shoulder Impingement: Causes and Solutions
Understand the concept of the shoulder impingement zone and the factors contributing to rotator cuff impingement and bursitis.
More info: Shoulder Impingement: Causes and Solutions
Frozen Shoulder: Overcoming the Stiffness
Discover how to unfreeze a frozen shoulder and regain a full range of motion through effective therapeutic approaches.
More info: Frozen Shoulder: Overcoming the Stiffness
Shoulder Dislocation/Instability: Seeking Stability
Explore the causes of shoulder dislocation and instability, and the fastest ways to promote healing and prevent future occurrences.
More info: Shoulder Dislocation/Instability: Seeking Stability
Can You Fix Shoulder Instability?
Find out about treatment options to address shoulder instability and regain stability in the joint.
More info: Can You Fix Shoulder Instability?
AC Joint: Identifying and Managing Injuries
Learn how to recognise an injured AC joint and what steps to take for proper care and recovery.
More info: AC Joint: Identifying and Managing Injuries
Swimmers Shoulder: Causes and Remedies
If you're a swimmer or engage in repetitive overhead activities, understanding the causes of swimmer's shoulder and how to prevent it is essential.
More info: Swimmers Shoulder: Causes and Remedies
We hope this comprehensive guide will prove invaluable in your journey to understand and manage shoulder pain and injuries. However, it's essential to consult a healthcare professional for personalised advice and treatment based on your specific condition. Let's dive into the world of shoulder health together!