Ankylosing Spondylitis
Article by Alex Clarke
What is Ankylosing Spondylitis?
Ankylosing Spondylitis (AS) is a condition that causes inflammation and pain in the spine and other joints, such as the hips, knees, ankles, shoulders, and between the sternum and ribs. In Australia, up to 2% of the population is affected, which is three times more common in men than women. Ankylosing Spondylitis typically affects people in their late teenage years or 20s, but it can start as late as 45. Poorly managed AS can permanently stiffen the spine, causing the bones to fuse and resulting in a stooped posture.
The cause of Ankylosing Spondylitis is unknown, although it appears to have a strong genetic link, particularly in people who carry the HLA-B27 gene. Unlike other common back pains, the disease typically presents without a specific cause. Symptoms of AS include back pain and stiffness that gradually increase, early morning stiffness, and pain that decreases after exercise and increases after rest. Ankylosing Spondylitis can also cause sleep disturbance, inflammation of the iris within the eye, and symptoms of inflammatory bowel disease.
If a physiotherapist suspects Ankylosing Spondylitis, they will refer you to a GP for further testing, including blood tests and imaging such as X-rays, MRI, or CT scans. If testing confirms Ankylosing Spondylosis, a rheumatologist specialising in diagnosing and managing AS will be consulted.
Treatment of Ankylosing Spondylitis involves medication prescribed by your GP and rheumatologist to control inflammation. Physiotherapy can also be essential in managing AS by reducing pain and inflammation and restoring normal joint range of motion, muscle length, neural tissue mobility, and resting muscle tension. Regular physical activity is one of the most effective treatments for Ankylosing Spondylitis. It is recommended to engage in a regular stretching program daily and do at least 30 minutes of moderate exercise on most days of the week.
What are the Symptoms of Ankylosing Spondylitis?
- Back pain/stiffness came on gradually.
- Early morning pain/stiffness, which reduces movement.
- Pain/stiffness improves after exercise and is worse after rest.
- Sleep disturbance, particularly in the second half of the night.
- Persistence of the above symptoms for more than three months.
- Pain is relieved for a time after a shower, bath or heat treatment.
- Inflammation of the iris within the eye. This may include pain in the eye or brow region, exposure to light, blurred vision or a reddened eye.
- The bowel lining may also be affected, causing symptoms of inflammatory bowel disease such as diarrhoea and bloating.
How is Ankylosing Spondylitis Diagnosed?
If your physiotherapist suspects ankylosing spondylitis, they will refer you to your GP for further testing, including blood tests and possibly imaging such as X-rays, MRI or a CT scan. If testing suspects Ankylosing Spondylosis, you are generally referred to see a rheumatologist specialising in diagnosing and managing AS.
Please consult your physiotherapist or doctor for specific advice.
What is Ankylosing Spondylitis Treatment?
Your GP and rheumatologist may prescribe medications to help control the inflammatory part of the disease. As well as seeing your GP or rheumatologist for check-ups, your physiotherapist plays an important role in helping you manage your ankylosing spondylitis.
PHASE I – Pain Relief
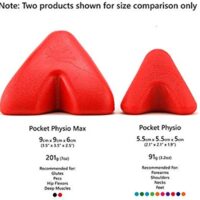
Your physiotherapist will use various treatment tools to reduce your pain and inflammation. These include heat, electrotherapy, acupuncture, de-loading taping techniques, and soft tissue massage.
PHASE II – Restoring Normal ROM & Posture
As your pain and inflammation settle, your physiotherapist will focus on restoring your normal joint range of motion, muscle length, neural tissue mobility and resting muscle tension.
Treatment may include joint mobilisation and alignment techniques, massage, muscle stretches and neurodynamic exercises, plus acupuncture, trigger point therapy or dry needling. Your physiotherapist is an expert in the techniques that will work best for you.
PHASE III – Restore Normal Muscle Control & Strength
Pain has an unfortunate side effect of ‘switching off’ your deep ‘core muscles. Researchers have discovered the importance of your muscle recruitment patterns with a normal order of deep, intermediate, and finally superficial muscle firing patterns in normal pain-free people. Your physiotherapist will assess your muscle recruitment pattern and prescribe the best exercises specific to your needs.
PhysioWorks has developed a “Core Stabilisation Program” to assist their patients in regaining normal muscle control. Please ask your physio for their advice.
PHASE IV – Restoring Function and Return to Activity
This stage of your rehabilitation aims to return you to your desired activities. Everyone has different demands for their bodies that will determine what specific treatment goals you need to achieve. For some, it is simply to walk around the block. Others may wish to run a marathon or return to a labour-intensive activity. Your physiotherapist will tailor your rehabilitation to help you achieve your own functional goals.
PHASE V – Long-Term Management
Ankylosing spondylitis is a condition that requires constant management. Sticking to a regular stretching plan specific to your stiffness helps get the most out of your body. Your physiotherapist will set you up with an appropriate stretching programme, monitor your symptoms, and make any adjustments as necessary.
The best advice is to keep active. Regular physical activity is one of the most effective treatments for AS. It is essential to engage in a regular stretching program daily and do at least 30 minutes of moderate exercise on most days of the week.
What Results Can You Expect?
Symptoms may flare and go into remission for many years. For others, the signs and disability may gradually worsen over time. Generally, people with AS can continue to work and perform daily activities. However, specific changes may have to be made to allow various positions and movements throughout the day.
Physiotherapy
Physiotherapy helps to provide pain relief and improve stiffness. Your physiotherapist can also provide you with a personalised exercise programme to help you manage your condition.
Surgery
Surgery is needed only if the disease has caused nerve damage in the spine or if joint damage is severe.
Massage
Many patients find that soft tissue massage therapy benefits pain relief, muscle relaxation, and reduced swelling. Would you please ask your physiotherapist if you would benefit from a massage?
Acupuncture
Acupuncture can be helpful for the relief of your pain. If you want to try some acupuncture, many of our therapists are trained in acupuncture. Please ask for their advice.
Weight-Loss
Carrying excessive body weight puts an extra load on your joints and muscles, predisposing you to increased pain.
General Exercise
General exercises are fundamental to keeping your body moving. If you enjoy a specific activity, please ask your physiotherapist if that activity will benefit your long-term health.
For this particular injury, other patients have benefited from the following activities: hydrotherapy, pilates, yoga, walking, swimming, cycling, or tennis.
Please consult your physiotherapist or doctor for specific advice.
Related Articles
- Spondylosis – This article discusses degenerative spine conditions and how they relate to lower back pain, including the role of physiotherapy in managing such conditions.
- Rheumatoid Arthritis – Offers insights into managing arthritis-related conditions, including Ankylosing Spondylitis, emphasising the importance of activity pacing, sleep health, and muscle treatment.
- Sacroiliac Joint Dysfunction (SIJ) – Details the causes, relief, and treatment for SIJ issues, which can be closely related to the symptoms and discomfort experienced by those with Ankylosing Spondylitis.
- Osteoporosis – Since bone health is crucial for individuals with Ankylosing Spondylitis, this article provides information on managing and improving bone density, which can be beneficial in the long-term management of the condition.
Article by John Miller
Understanding Arthritis-Related Conditions
An Overview
Arthritis is a prevalent and diverse group of conditions affecting millions worldwide. It encompasses many disorders characterised by inflammation and joint pain, often leading to stiffness, swelling, and reduced mobility. Arthritis can significantly impact a person's quality of life, affecting their ability to perform daily tasks and engage in physical activities.
This article aims to provide a comprehensive overview of arthritis-related conditions, focusing on both rheumatoid and osteoarthritis. By understanding these conditions' causes, symptoms, and treatment options, individuals can make informed decisions about managing their joint health and seek appropriate medical guidance.
Arthritis Overview
In this article, we will explore the fundamental aspects of arthritis, including its definition, common symptoms, and risk factors. By establishing a clear understanding of what arthritis entails, readers can grasp the broader context before diving into specific subtypes.
Rheumatoid Conditions
This article delves into rheumatoid conditions, encompassing autoimmune disorders primarily affecting the joints. We will provide an overview of each condition, highlighting key characteristics, diagnostic approaches, and available treatment modalities. The rheumatoid conditions covered in this article include:
- Ankylosing Spondylitis,
- Fibromyalgia,
- Lupus,
- Psoriatic Arthritis,
- Rheumatoid Arthritis.
- What is a Rheumatoid Physiotherapy?
Osteoarthritis Conditions
Osteoarthritis, the most common form of arthritis, is the focus of this section. We will delve into its definition, underlying causes, risk factors, and prevalence. Additionally, we will explore specific osteoarthritis conditions.
Spinal Arthritic Conditions
Peripheral Joint Arthritis
By dividing the information into these sections, we aim to provide readers with a well-structured and informative resource. Each section will delve into the specificities of the respective conditions, including their impact on different parts of the body, available treatment options, and strategies for managing symptoms. Whether you seek general knowledge or are personally affected by arthritis-related conditions, this article is a valuable guide to navigating this complex field.
Please note that while this article provides a comprehensive overview, it is not a substitute for professional medical advice. Individuals experiencing symptoms or seeking specific treatment recommendations should consult with qualified healthcare professionals for personalised care.
Article by John Miller
Understanding Osteoarthritis
Osteoarthritis, commonly referred to as degenerative arthritis, stands as one of the most prevalent forms of arthritis.
Joints, over time, exhibit signs of wear and tear: the joint cartilage thins out, extra bony spurs develop in response to stress, and joint mobility diminishes. In advanced stages, osteoarthritis can become not only painful but also limiting in function and mood.
Exploring Osteoarthritis Management
Regrettably, a cure for osteoarthritis remains elusive. Nevertheless, there are more effective methods to manage the condition and slow down the degenerative process. By embracing these improvements, you can make your life smoother and more comfortable. A crucial component of this approach is physiotherapy, which plays a pivotal role in reducing osteoarthritis-related discomfort, enhancing comfort, and maintaining your activity levels.
Validating with Research
Numerous studies underscore the benefits of physiotherapy in alleviating pain and mitigating the disability linked to arthritis, especially in cases of knee osteoarthritis. (Source: http://dx.doi.org/10.1136/bjsports-2016-096458)
Empowering through Expert Guidance
To rediscover the joy of life, seek the insightful counsel of your physiotherapist today!
Navigating Osteoarthritis Diagnosis
The most straightforward test to confirm osteoarthritis remains an X-ray. A skilled practitioner can often make a reliable assessment of your condition upon examination.
Impact on Ageing Individuals
As we age, most of us inevitably encounter some degree of osteoarthritis. The wear and tear on our joints can result from various factors, including aging, injury, prolonged microtrauma, joint overuse, or excessive weight. This can lead to lasting changes in the bones, even in the absence of painful symptoms.
The extent of suffering varies, ranging from mild or occasional pain triggered by increased use or minor injury, to those who remain symptom-free and others who experience constant debilitating pain.
Weight-bearing joints like the hips, knees, ankles, feet, and spine are commonly affected. However, osteoarthritis can target any joint in the body, with hands and shoulders also being frequently affected. While severe cases might necessitate surgery, the majority respond positively to the combination of physician-prescribed physiotherapy and medication.
Recognising Osteoarthritis Signs
Osteoarthritis might be suspected if you encounter any of the following:
- Intermittent joint pain or tenderness
- Morning stiffness, particularly pronounced
- Swelling or distortion of the joint
- Detectable warmth and redness in the joint
- Challenging joint movement
Holistic Osteoarthritis Care
For guidance on your osteoarthritis diagnosis, self-help strategies, or the most suitable treatment, reach out promptly to your physiotherapist or a trusted healthcare professional.